An 88 year old lady (Agnes) presents to the acute medical unit. She has been having problems with dizziness and fatigue over the past few weeks. She presents following a fall. You take a history
Presenting complaint – Fall – ? cause
HPC- She reports falling following standing from a chair. She remembers feeling a little dizzy prior to her fall. She is unsure if she lost consciousness -if she did it was only for a few seconds. She had no chest pain and no palpitations prior to this. She reports a sore knee but no other injuries. No signs of infection
PMH – Hypertension, osteoporosis, previous breast cancer -treated
Medications – Bendroflumethiazide, amlodipine, adcal D3
NKDA
Social – non-smoker, minimal alcohol intake, lives alone with no package of care
She is convinced that she must have tripped over something but there was nothing on the ground. She is keen to get home.
Are there any other questions you would to ask?
have a think before you reveal what we would suggest.
We need to go into the fall further. Certain characteristics may help you to determine what sort of an event this was
Cardiovascular – She has denied any preceding chest pain or palpitations. She has also denied any head injury or facial injury. These 2 patterns of injuries are more typical of someone blacking out as they have not been able to put their hands out to protect their face. It would be interesting to know if anyone in the family had any cardiovascular issues however at this age any cardiovascular presentation is likely due to degeneration over years
Neurological – We would be thinking seizure here. The most useful thing would be to have a witness to the fall, however in this case that is unavailable. Other questions which would be useful to ask are:
- Did you injure yourself?
- Did you bite your tongue?
- Any incontinence – bladder or bowel?
She denied any of these features
Other
It would be useful to know about anything that would lead you to think this was a trip or balance issue. This would be asking about any rugs or object on the floor that someone could have tripped over.
Changes in eyesight recently or new glasses. Poor vision can increase likelihood of falls.
Any recent changes to medication? Some medications can predispose to falls, most commonly anticholinergic medications, analgesics, anti-hypertensive medications
She tells you she has had some problematic blood pressure readings lately and has been told to try taking 2 of her amlodipine tablets instead of one.
Before moving on with the case have a think. You should have enough information to be forming a differential diagnosis for this lady’s fall.
Write down your top 3 differential diagnoses and see if they fit with the ones we have suggested.
- Postural hypotension
- Trip over an object as yet unknown
- Balance abnormality
You continue with your assessment of this lady and move on to examination.
| Cardiovascular – Warm, well perfused – Good volume radial pulses, No radial/radial delay – JVP not visible -HS 1+2+0, No Murmurs -Mild lower leg swelling | Respiratory -Comfortable at rest, talking in full sentence – No signs of cyanosis – Normal expansion – Resonant to percussion – Chest – good AE throughout |
| Abdominal – Abdomen moving with respiration – No scars, hernia or oedema visible – Abdomen soft and non-tender to light and deep palpation – No palpable organomegally – BS audible | Neurological – No abnormalities on examination of cranial nerves – Normal power (5/5) and tone in upper and lower limbs – Sensation -intact throughout – co-ordination – can walk without abnormality – Rhomberg’s test negative – reflexes intact |
| Musculoskeletal – Bruising and swelling to left knee – Full RoM and able to weight bear on leg | GCS 15 AMT 10/10 BP 148/85, HR 76, Sats 99% RA, RR 17, T 36.8 |
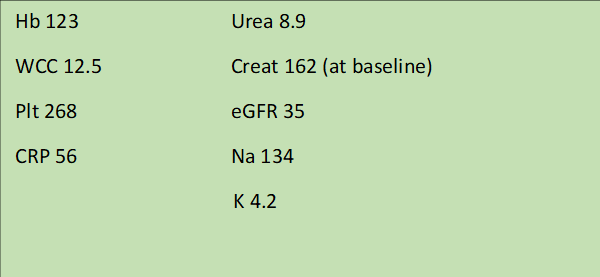
She has already had blood tests taken during this presentation