As we all know, hypertension is associated with significant morbidity, predisposing to the development of hypertensive nephropathy, cardiovascular disease, stroke and poorer outcomes in certain illnesses (Covid-19 as an example). Therefore control of hypertension is important to stop the progression.
Roughly speaking there are 4 main drug classes used in the management of hypertension. These are
- ACE – inhibitors
- Calcium Channel Blockers
- Diuretics
- Beta-Blockers
This page hopes to explain a little about the common classes of medications, when they are required and some of their most common side effects.
ACE -Inhibitors
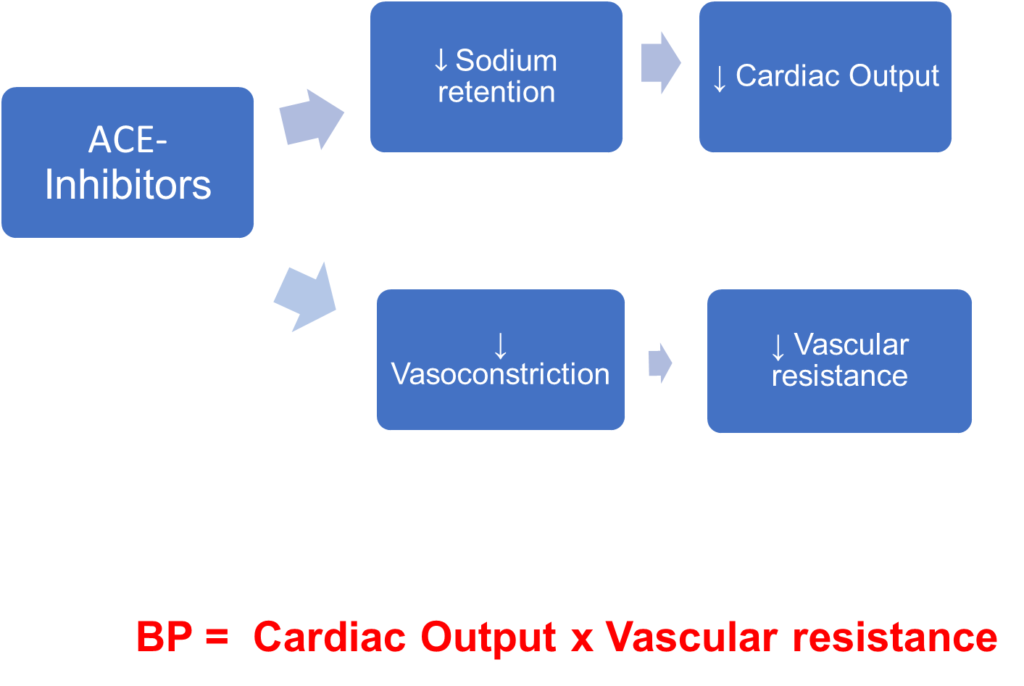
ACE- Inhibitors (or angiotensin converting enzyme inhibitors to give them their Sunday name) are a commonly utilised medication in the management of hypertension.
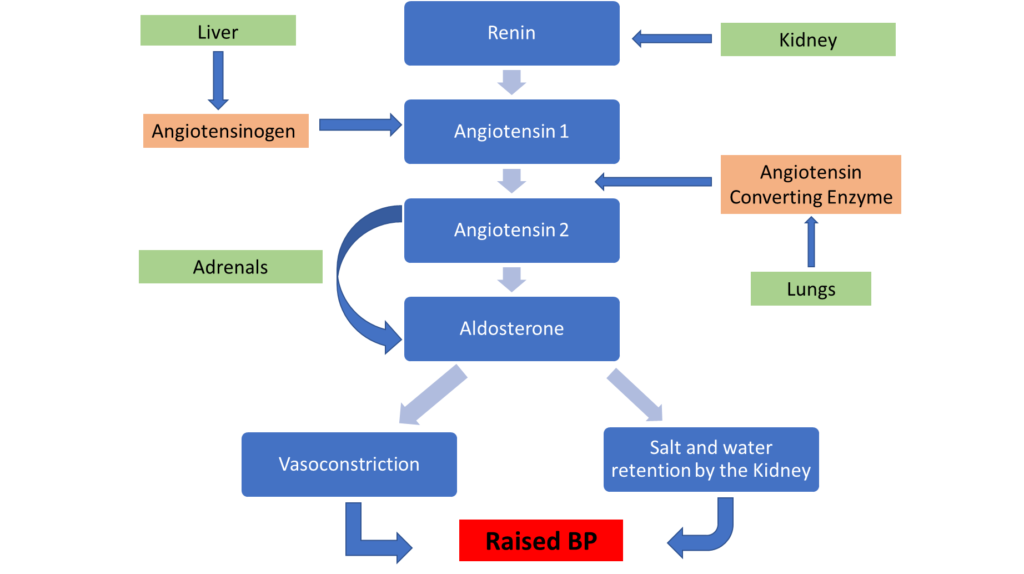
Above is the renin angiotensin aldosterone system ACE inhibitors work between the stage of Angiotensin 1 which is inactive being converted to the active form of angiotensin 2. This breaks the chain and thus ultimately lowers the blood pressure.
ACE- inhibitors = lisinopril, ramipril, catopril
Who do you think could benefit from ACE-inhibitor therapy?
These medications are commonly prescribed to diabetic patients. They help to reduced proteinuria and thus progression of renal disease. They also are used as part of secondary prevention for cardiovascular disease which diabetics and those with renal disease are at increased risk of developing.
Again these medications are commonly used in heart failure due to there role in reducing vasoconstriction and decreasing systemic vascular resistance.
While you may see some older individuals on ACE-inhibitors, they are not first line and if you are treating an individual with a new diagnosis, this would not be the first medication you would prescribe. This is due to decreased renin production as individuals age.
Whilst ACE-Inhibitors are useful in many causes of chronic kidney disease it is important to remember that it is contraindicated in patients with renal artery stenosis.
Black individuals, along with the elderly, tend to have decreased renin production so are not as useful in the management of hypertension in these individuals.
What are the side effects of ACE-inhibition?
As with all medications, ACE-inhibitors come with side effects. Below are listed a range of side effects. Select those that apply.
This is a possible complication of ACE-inhibition in people who have renal artery stenosis. This is due to the fact that glomerular filtration in those with renal artery stenosis is maintained by angiotensin-2 mediated constriction of the efferent arteriole which ACE-inhibition prevents. For this reason all individuals should have renal function monitoring following initiation of ACE-inhibition 1-2 weeks after implementation.
This is a common side-effect of ACE-inhibitors. It is due decreased degradation of bradykinin in the body (Angiotensin converting enzyme is also needed to convert bradykinin to an inactive peptide). For most individuals switching to an angiotensin 2 receptor blocker can overcome this side effect
This is another side effect of ACE-inhibition which occurs in 0.1% – 0.35% of recipients (higher percentage in black individuals). This again occurs due to decreased bradykinin degradation, increased substance P and increased active Bradykinin metabolites. This leads to vasodilation and increased vascular permeability and ultimately angioedema
This is not a side effect of ACE-inhibition but can be attributed to other classes of antihypertensives.
Yes. Remember that Aldosterone works on the sodium potassium pump drawing potassium out and into the urine. With ACE -inhibition there is less aldosterone and thus plasma potassium is elevated.
As a last note on ACE-inhibitors, due to their side effect profile, it is important to withhold these medications if a patient is in a dehydrated state or is unwell. You should also be advising patients that these should be withheld if vomiting or unwell in order to prevent complications from profound hyperkalaemia or acute kidney injury.
Calcium Channel Blockers
Calcium channel blockers are the first choice medication in black and older individuals. They work by decreasing calcium influx into cells leading to decreased vascular contractility (vasodilation) and by this mechanism blood pressure is reduced
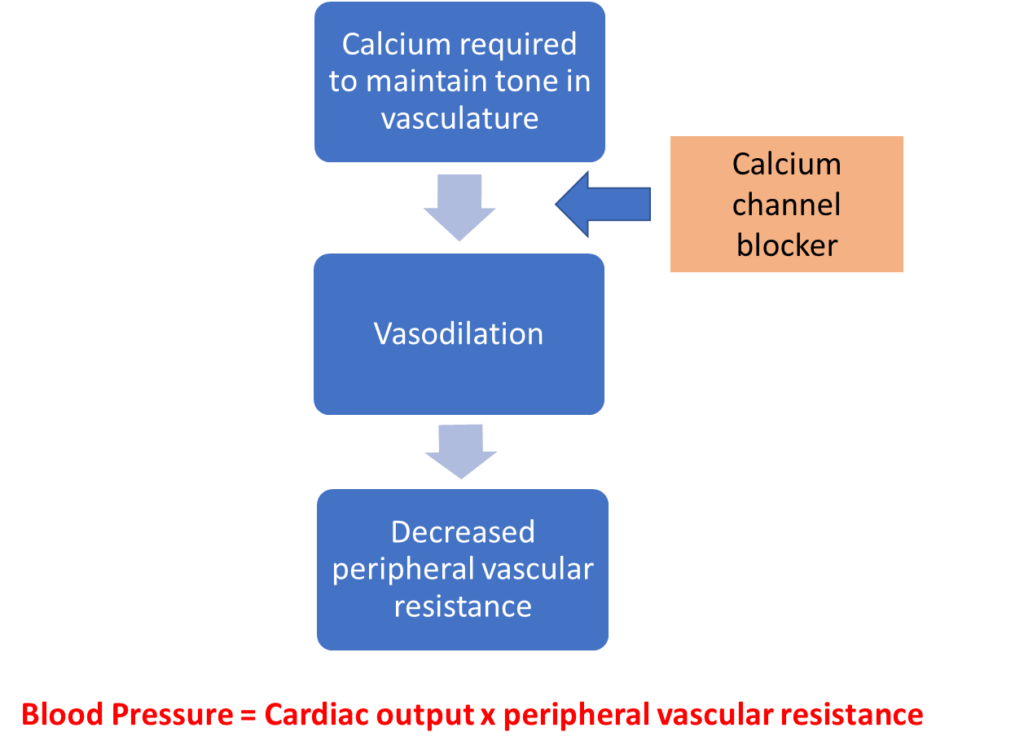
Blood pressure is therefore reduced as cardiac output remains the same and vascular resistance drops.
Calcium Channel blockers = Felodipine, nifedipine, amlodipine, diltiazem, verapamil
Who may benefit from taking a calcium channel blocker?
As calcium channel blockers lead to vasodilation and decreased vascular resistance and arterial pressure. They are there effective in reducing cardiovascular and cerebrovascular disease.
Calcium channel blockers are used as a first choice in the treatment of hypertension in those over 55 years.
As calcium channel blockers are negatively inotropic and chronotropic, they should be avoided in people with impaired left ventricular function.
Calcium channel blockers can be useful to treat individuals who have Raynaud’s due to their action in preventing vasoconstriction.
Side Effects
Common side effects of calcium channel blockers include ankle swelling – particularly with amlodipine and this tends to resolve with discontinuation of the medication. There are some further side effects. Select those which are correct
This is a common side effect due to vasodilation in the cerebral arteries.
Renal impairment is not commonly seen due to calcium channel blockade however note that it can occur due to hypotension.
This can occur due to reduced formation of and conduction of impulses through the cardiac conduction system which can lead to bradycardia.
As stated above Calcium channel blockers can lead to peripheral oedema but not to angioedema.
Bronchospasm is not associated with calcium channel blockers but is associated with another form of antihypertensive.
Thiazide Diuretics
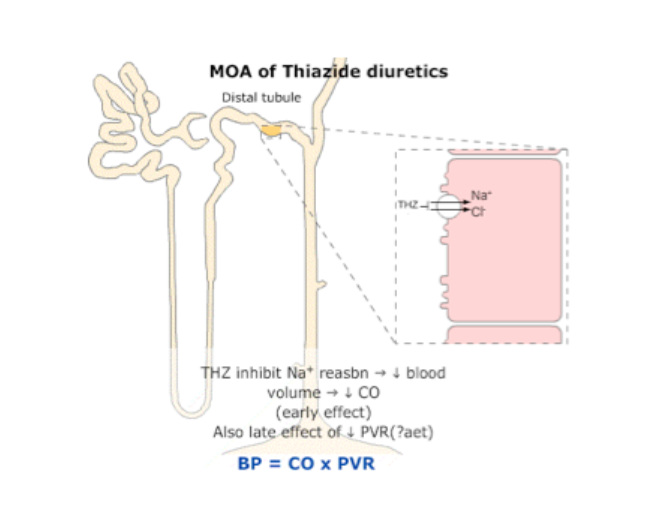
Therefore blood pressure is reduced due to decreased cardiac output from reduced sodium reabsorption.
Thiazide diuretics = bendroflumethiazide, chlorthalidone, indapamide
Thiazides are another agent that can be used in the management of hypertension in those older than 55.
Select further which of these further possible uses of Thiazide diuretics are correct.
As stated above this is not true. Along with calcium channel blockers these can be thought of as first line agents for those over the age of 55years. However these should be used in caution in those with diabetes, renal disease and heart disease where there are better first line options.
These medications can also be used in the management of hypertension in individuals in black people, those >55 years and those with obesity.
While thiazide diuretics are useful in the management of hypertension, loop diuretics are better to manage fluid retention associated with heart failure.
Which of the following are side effects of Thiazide diuretics?
This is associated with calcium channel blockers and thiazides being diuretics may help to resolve any oedema that is present.
Due to their mechanism of action, these medications can cause hyponatraemia. If hyponatraemia is recurrently low it may mean that a different agent is required.
This is not the case as thiazide diuretics cause hypocalciuria. Loop diuretics can lead to hypercalciuria as they increase urinary calcium loss.
Thiazide diuretics can cause both hyponatraemia and hypokalaemia due to increased loss of sodium and water in the collecting duct. They can also lead to metabolic alkalosis.
This is associated with ACE-inhibition not thiazide diuretics.
As with ACE inhibitors, you should consider withholding these medications in any dehydrating illness.
Beta-Blockers
Beta blockers = bisoprolol, metoprolol, propranolol, labetalol
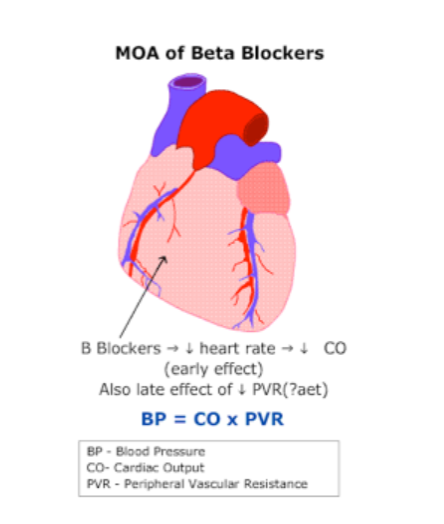
Beta blockers work to block beta receptors on the cell surface. The beta receptors activate the sympathetic nervous system. Blocking these receptors therefore lead to decreased heart rate and decreased cardiac output. They therefore reduce blood pressure.
Who could benefit from Beta blocker therapy?
Beta blockers ( particularly propranolol) are used in the management of people with migraine
Beta blockers can trigger bronchospasm and as such should be avoided in individuals with a history of asthma.
Beta blockers can be used to relieve some of the symptoms of anxiety and may be used in these individuals.
Beta blockers reduced myocardial oxygen demand and thus reduce anginal symptoms and may prolong life in individuals with ischaemic heart disease.
These are appropriate treatment for this group of individuals if they are Caucasian. As stated before there are other medications more suitable for those who are black.
Bronchospasm, as stated above, can occur with beta blocker therapy, there are other side effects that you should be aware of.
Which of the following are side effects of beta blockers?
There is a slight increase in incidence of erectile dysfunction in those who are taking beta blockers.
Beta blockers can worsen vasospasm in those with Raynaud’s phenomenon and also can worsen perfusion critical limb ischaemia. They do not however cause peripheral vascular disease.
ACE-inhibition, rather than beta-blockade is associated with cough.
This can occur due to beta blockers being negatively chronotropic
Beta blockers can impair hypo awareness alone and as such there is a relative contraindication to them in diabetic patients. Combined with thiazide diuretics there is also an increased risk of developing diabetes.
This page has covered the main medications used to manage hypertension. There are other medications that you may see used and you should familiarise yourself with these in further reading (Angiotensin 2 receptor blockers etc).
For further information about implementation of antihypertensive agents the NICE guideline on hypertension provides a good summary.
