Describing recognition and early management of AKI. (More advanced info from Specialist page).
Early Recognition (KDIGO criteria):
AKI 1: creatinine rise from baseline of 1.5x or 26.5 micromol/l, and/or oliguria (urine output <0.5ml/kg/hr for >6hrs)
AKI 2: rise of 2-3x baseline
AKI 3: rise of >3x baseline or >354 micromol/l, or need for RRT
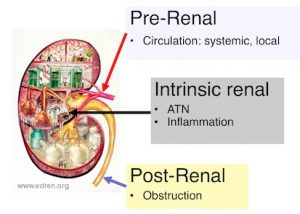
Consider potential causes
- Sepsis
- Hypoperfusion
- Cardiac/liver failure
- Haemorrhage
- Dehydration
- Drugs or Contrast
- Obstruction
- Renal disease
- e.g rhabdomyolysis, glomerulonephritis, interstitial nephritis, myeloma
Assessment/Management
1. Correct hypovolaemia
- Use small fluid boluses (250ml) of crystalloid initially (see fluid therapy)
- Regularly reassess JVP, peripheral perfusion, BP, urine output
2. Address hypotension
- If persistent once euvolaemic, consider CVP monitoring +/- vasopressors (HDU/ ITU?)
3. Manage hyperkalaemia
- Hyperkalaemia protocol
4. Review drugs
- Stop any drugs which may contribute
- Stop antihypertensives if BP low
- Review all drug dosages in renal impairment
5. Urinary tract ultrasound
- Consider if clinical suspicion of obstruction/abnormal renal tract
6. ALERT SENIOR STAFF EARLY
Required actions
1. Senior review
2. Updated renal function
3. Check historic renal function
4. Fluid balance assessment
5. Drug chart review
6. Urine dip (+/- protein:creatinine ratio)
7. Check acid/base (TCO2 /H+/pH)
8. Consider urinary tract ultrasound
Consider specialist (nephrology) referral if:
- Clinical suspicion of intrinsic renal disease (even if mild AKI)
- Proteinuria +/- haematuria
- Absence of clear precipitant of AKI
- Symptoms/signs suggestive of systemic disease
- e.g. rash, arthropathy, pulmonary infiltrates
- Progressive renal impairment
- Renal transplant
- Refractory pulmonary oedema
- Refractory hyperkalaemia (> 6.5 mmol/L)
- (Refractory acidosis (H+> 60 nmol/L; pH<7.2))
- (Background CKD 4/5)
AKI outcomes
AKI is a smoke alarm! It is associated with:
- Longer hospital stay
- Increased mortality
But most patients don’t die of renal failure. They die from their underlying condition.
And remember that too much fluid is a bad prognostic feature in AKI.
Further info
Fluid therapy – our page on the principles and practice.
AKI (specialist) – also has pointers to other sources of info, including for patients
Acknowledgements: Ailish Nimmo was the main author for this page, which was created in November 2017. Date last modified shown in footer.