Active conservative treatment of patients with severe uraemia was started in the early 1950s before dialysis was available by Drs J.S. Robson and C.P. Stewart (RIE clinical biochemist) and their team, who worked in the Department of Therapeutics at the RIE, had interests in endocrine disease and metabolic medicine. Their research interests were in fluid and electrolyte problems, including those that are related to renal function, adrenal and pituitary function. Work was carried out in Professor Derrick Dunlop’s metabolic ward. Patients with renal failure were put onto a low protein, low salt, low potassium and high calorie diet that was said to enable the patient to survive while the kidneys recovered from ‘acute urinary suppression’ (acute tubular necrosis). While this treatment was undoubtedly an advance, there were many patients who did not survive it. More info
Reports of success with dialysis began to spread during the 1950s, and there was a growing interest in renal medicine. Previously fit healthy men who had the ability to get through an acute illness needed something else to support them while their kidneys failed. The use of dialysis during the Korean War (1950-1953) helped to establish its place. By the early 1960s, dialysis for patients with acute renal failure was becoming established in Western countries.
At about the same time, knowledge of renal diseases was being helped by the introduction of techniques for renal biopsy (being able to sample the kidney and look at it under the microscope). This was first introduced in Edinburgh in 1956. The first renal biopsy in the world was performed in 1901, but the first percutaneous needle renal biopsy was performed by Ball in 1934. It required a pathologist with specialised knowledge in kidney tissue. Dr Mary MacDonald was in charge of the pathology side of renal biopsy at the time. Nephrology was growing as a discipline.
Contents
- Haemodialysis in Edinburgh: How it all began
- The first artificial kidney in Edinburgh
- The Kolff-Travenol twin-coil artificial kidney: technical aspects
- Outcome for patients with acute renal failure treated by haemodialysis
- The cost of dialysis
- The Renal isolation unit (RIU): 1962
- Reaction to haemodialysis for patients with acute renal failure
- The Renal Unit in the 1960s, 1970s and 1980s
Haemodialysis in Edinburgh: How it all began
In 1958, Dr Rae Gilchrist (consultant cardiologist at the Royal Infirmary of Edinburgh) was impressed by Professor Nils Alwall’s work after attending a conference in Sweden. Dr Gilchrist suggested that an artificial kidney should be installed in the RIE. It was noted in the Minute of Meeting of the Medical Committee (24/3/1958) that “the Committee agreed to recommend that the action taken in this matter be homologated” after hearing a report by Dr Gilchrist on the desirability of having an Artificial Kidney Unit at the Royal Infirmary of Edinburgh (RIE) (Minutes of the board of management and committees, RIE, No. 8, 1958).
Professor James Robson and Professor Hugh Dudley, who were both senior registrars at the time, were asked to visit the three places in the UK where the use of artificial kidneys was established: The Royal Air Force Renal Unit at Halton, Hammersmith Hospital in London, and Leeds General Infirmary. The purpose of visiting these artificial kidney units was to obtain information about the design and operation of artificial kidneys. The secondary aim was to gain information on the value of this form of therapy.
A modified version of the original Kolff rotating drum artificial kidney, the Kolff-Brigham kidney, was used in Leeds. A further modified version (Usifroid, France) of this was used at Hammersmith. A newer Kolff-Travenol, twin coil artificial kidney was used at Halton. Group-Captain Jackson, medical specialist at Halton, spent two days demonstrating how haemodialysis worked and the exciting results of haemodialysis. The artificial kidney unit at Halton impressed the visitors the most.
| Report on the United Kingdom Artificial Kidney Units (1958) | |||
 |
Competing machines in 1958. A rotating drum kidney, the Kolff-Brigham, as used in Leeds. Better picture |  |
Competing machines in 1958. The twin-coil Kolff-Travenol machine, as used at RAF Halton. Better picture |
Robson and Dudley reported:“The Kolff-Travenol pressure-dialyser possesses material advantages over the other two (dialysers) in respect of ease in sterilisation (i.e. disposable coil), ease of setting up and running, adaptation to ultra filtration and dialysis and, in our opinion, safety in the method and accuracy of the control of the blood volume in the machine. The Kolff-Travenol machine is more compactly made and more easily maintained than the other two. It is very considerably cheaper in the capital cost, though more expense is involved in each dialysis” (Report on the visits to the artificial kidney units in UK for the Royal Infirmary of Edinburgh by JS Robson and HAF Dudley, August, 1958).They concluded:“The Kolff-Travenol Artificial Kidney with disposable coils and incorporating ultra filtration and dialysis is the machine which combines the most advantages. Its simplicity of preparation and operation and its intrinsic safety are outstanding. It has the additional advantage of relative cheapness. For the operation of dialysis two doctors and two nurses are required. One of the nurses should be senior and preferably have operating theatre experience. One other member of the medical staff should be able to run the machine. A full time biochemical technician is necessary. The room in the Clinical Laboratory suggested for the artificial kidney when suitably equipped, would be adequate for the purpose.” |
|||
 Click here to view the full report (28k pdf file) |
|||
It had been stated in the Memorandum regarding the Artificial Kidney for the RIE (March 1958) that an artificial kidney in RIE could be used to treat cases of poisoning and for the treatment of surgical patients, obstetrical patients and medical patients who develop acute renal failure. There had been 34 deaths in 1957 in the RIE due to conditions where the value of an artificial kidney had been established, including 7 cases of poisoning, 18 surgical cases, 6 medical cases and 3 obstetrical cases, illustrating the need and potential benefits of possessing an artificial kidney, justifying the proposal for its purchase. In 1958, It was estimated that a Kolff-Travenol Twin Coil Kidney would cost US$ 1538, and 100 disposable coil kidneys would cost US$ 5900.
The decision to purchase a Kolff-Travenol artificial kidney for Edinburgh was made due to its advantages over the Kolff-Brigham machine.
| There was no significant opposition to purchasing the artificial kidney as medicine was expanding quickly at the time, and the machine was not very expensive.” (Dr A Lambie) |
| Document Letter from the secretary of the medical staff to the secretary of gynaecological staff, stating that the provision of a modern artificial kidney in the Royal Infirmary would be desirable as a therapeutic weapon in the treatment of renal disease and extra-renal disease such as barbiturate poisoning. From the Lothian Health Service Archive, with permission. Click to view |
The first artificial kidney in Edinburgh
The first artificial kidney unit in the RIE was set up in a small room converted from 3 clinical laboratories to accommodate the new Kolff-Travenol twin coil artificial kidney. This was known as the Artificial Kidney Unit (AKU). The alterations necessary for providing accommodation for the AKU in the south end of room B12 would cost about £1000. The Works and Buildings Committee recommended approval of the first stage of work after discussion on 21/10/1958 (Minute of Meeting of the Works and Buildings Committee, book no 8). It was reported in the Minute of Meeting of the Works and Buildings Committee, 18/11/1958 that “the board of Trade Import Licences for the Artificial Kidney Unit had now been received and arrangements were in hand for the necessary letter of credit to be sent to the Firm. Despatch was promised two weeks after the receipt of the letter of credit, and it could, therefore, be estimated that the apparatus would be received at the Royal Infirmary of Edinburgh about the middle of January (1959)”. (Minute of Meeting of the Works and Buildings Committee, 21/10/1958, book no 8).
In the progress report of the Works and Buildings Committee in May 1959, “the partitioning, the new ceiling, lighting, jointless flooring, sanitary and other fittings had been completed, or were nearing completion, and painting work was in hand. Every effort was made to have the unit finished by May 20th.” (Minute of Meeting of the Works and Buildings Committee, 19/5/1959, book no 9).
The Artificial Kidney Unit was opened on 20 May 1959 by the Earl of Wemyss, then Lord High Commissioner to the General Assembly of the Church of Scotland, accompanied by a member of his Bodyguard of Archers. He regretted that it was not possible to fill the 100-litre tank of the artificial kidney with champagne to mark the occasion! (Lambie AT, 1990).

The first patient was dialysed 2 days after the opening of the AKU in May 1959. A young man presented with biliary sepsis, Escherichia coli septicaemia, oliguria and uraemia, who was unfit for the necessary surgery (Lambie AT, 1990). He was dialysed, and biliary drainage was subsequently performed. He made an excellent recovery, illustrating in thischart (contemporary chart provided by Dr A Lambie).
Nine patients were dialysed in the first 6 weeks of the AKU’s opening (between 20/5/1959- 4/7/1959) (RIE annual report 1958-59). The RIE annual report for 1959-1960 recorded that the AKU, established in the Department of Therapeutics and Clinical Medicine, had carried out 65 dialyses on 50 patients since its establishment in July, 1959, and had saved many lives.
The AKU received patients referred from many parts of Scotland, even the Orkney Isles. Haemodialysis in those days was lengthy, often taking up to 6 hours in the cases of uraemic patients, and 8 hours in poisoned patients. Dialysis often took place at night when severely uraemic patients who came from a distance were admitted late in the day.
The Kolff-Travenol twin-coil artificial kidney: technical aspects
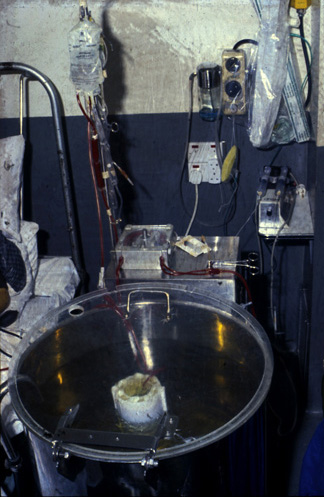
| The dialysis machine consisted of a twin coil in a big cylindrical steel tank that could hold about 100 litres of water. There was a blood pump in the front, a heater that maintained a constant dialysate temperature, a re-circulation pump and a pump for emptying the dialysate.
Dialysis with the Kolff-Travenol twin-coil artificial kidney was a labour-intensive procedure. Hot and cold water was mixed to the correct temperature as the heater was only able to maintain a given temperature. Salts including sodium chloride, calcium acetate, potassium acetate, sodium bicarbonate, glucose and lactic acid were added to the water to make up the dialysate (the “bath”). The potassium concentration was altered according to each patient’s requirements. An extract from one of the calculations for a hyperkalaemic patient read: “only 20 grams of potassium acetate was added to each Kolff bath, giving a potassium concentration of approximately 3 mEq/L.” Patients with severe acidosis were dialysed against a bath containing a higher than normal concentration of bicarbonate. The amount of bicarbonate salt required would be worked out and bicarbonate powder would be weighed and added to the bath. The conductivity of the electrolyte solution was checked. The dialysate bath was emptied and changed every 2 hours. Medical staff supervised patients going on dialysis. Other tasks for the medical staff included monitoring the blood pressure of patients, weighing patients (3 times during dialysis using weigh-beds), taking blood for analysis, and doing certain laboratory analyses. |
| To take fluid off from patients, there was not the luxury of today’s machines that incorporate volumetric controlled ultra-filtration, where one can dial into the machine what weight the patient has to lose, and the machine works out the pressure. The Kolff machine did not record fluid removal. Doctors set the pressure on the machine manually. Gate clips on venous lines were tightened till the desired weight is taken off. The patients were weighed continually during dialysis using a “weigh bed”. It was difficult to accurately get to the desired weight – a ‘hit and miss’ process.
Safety features for the machine were very limited. There were no alarms, temperature and pressure monitoring, full function checks, blood leak detectors, ultra-filtration pumps or air embolism detector. The machine had no mechanism to record changes in pressure. If a needle fell out the patient’s blood could be rapidly pumped onto the floor. The cover over the tank did not close properly when the coil was in place, so fluid could splatter everywhere. |
A considerable amount of the doctors’ time was taken away from other clinical duties. The need for more frequent, shorter dialysis for patients with acute renal failure (ARF) could not be met until a team of nurses was specially trained in the mid-1960s primarily to look after patients suffering from chronic renal failure (CRF) who required dialysis. Infrequent vigorous dialysis was gradually phased out. More frequent and better-monitored dialysis was possible from 1966 onwards. Blood urea levels were maintained at a lower level due to frequent dialysis. Patients’ diets improved as frequent dialysis imposed fewer restrictions on the diet. This allowed better nutrition, both orally or parenterally. The policy of using short frequent dialyses in Edinburgh was not adopted in all the dialysis units across UK.
The Kolff twin coil artificial kidney was kept in use in Edinburgh till the late 1980s despite being a labour-intensive operation, since the bicarbonate buffer was more suitable for patients with acute renal failure and also produced less changes in blood pressure.
Outcome for patients with acute renal failure treated by haemodialysis
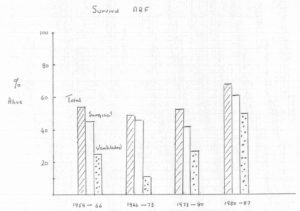
Haemodialysis gave very exciting prospects, as the mortality from severe ARF had previously been almost 100%. As it was a relatively new procedure, the outcome and possible complications were not clear. As a result, patients were only dialysed if their chance of dying due to uraemia was greater than the possible risks of haemodialysis. It was thought that there was a point in the natural history of ARF at which the patient appears to “pass beyond the limit of no return”. (Robson JS, 1961). In Professor Robson’s experience, serious prognostic signs at the time included focal or generalised neurological features and severe acidosis. This meant that the ideal time for dialysis had past.
In the early days, patients with a blood urea of over 300 mg % (i.e. 35.7 mmol/L) would be dialysed for 6 hours, producing a big change in the blood biochemistry, which was thought to be desirable. Subsequent research in Edinburgh, Glasgow and London showed that large gradients of hydrogen ions, bicarbonate ions and urea developed across the blood brain barrier after such dialyses (Lambie et al, 1965). The hydrogen ion concentration in the cerebrospinal fluid rose in some cases where large changes had been made in the concentration of bicarbonate in the extra-cellular fluid and the patient became hyperpnoeic. This state of disequilibrium was associated with clinical deterioration. The consideration of purchasing a more powerful rotating drum artificial kidney, which could produce even larger changes in the composition of the extra-cellular fluid in a short time, was therefore ruled out.
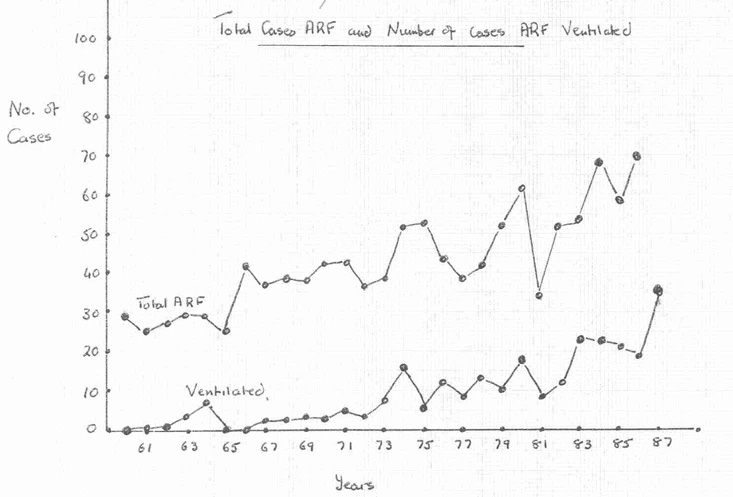
In the 1960-1961 RIE report, 50 patients were dialysed that year. The workload of the AKU increased steadily and in the year 1961-62, 66 dialyses were performed on 50 new patients (1961-62 RIE annual report). 47 patients were dialysed the following year (1962-63 RIE annual report).
| In the first year of HD, survival was about 52%. Patients usually died of non-dialysis-related problems such as the underlying condition, severe shock or severe super-infection. They did not die of biochemical disturbance. As early as 1959, it was the policy in Edinburgh to perform daily blood cultures and swabs on patients with infections. Narrow-spectrum antibiotics were used with the view to prevent the emergence resistance organisms.The percentage survival for dialysed patients with acute renal failure gradually improved from 59% in 1959 to 69% in 1987. This occurred despite increasing complexity and severity of the cases. |
The cost of dialysis
| RIGHT: Some equipment requests for the Artificial Kidney Unit, with costs, in the late 1950s and early 1960s (RIE minute of meetings, 1958-62)
In addition to the cost of the artificial kidney machines and staff employment, other expenses related to dialysis were often expensive. Some of the items that were applied for purchase are shown in this table. The renal unit had to “compete” with other units in the RIE for funds to buy equipment. Funding was allocated according to the necessity and cost of the equipment. In the Minute of Meeting of the Establishment Committee (19/04/1962) was a request for telephone installation in the home of the biochemist attached to the AKU, Mr John Cowie, in case of emergencies in order to avoid having to send taxi or a police car for him. Patients who were transferred from places far from Edinburgh often arrived late in the afternoon, by which time the biochemist had gone home. The biochemist was important to make estimations every 2 hours during dialysis. The sodium, potassium, urea, bicarbonate, blood pH and pCO2 was measured in a laboratory just outside the AKU, and these results determined changes to the composition of the Kolff bath. It was decided after discussion by the committee not to approve this request. |
|
The Renal isolation unit (RIU): 1962
Patients with acute renal failure were often very susceptible to cross-infection; nursing in isolation was thought to be beneficial. Initially this was carried out in a room in the Clinical Laboratory which had previously been used to see out-patients. Subsequently the Renal Isolation Unit was constructed. It was reported in 1962 (1961-62 RIE annual report) that wards 23 & 24 had been completely renovated and modernised and an isolation unit (later known as 21A) for the artificial kidney patients incorporated in ward 23. This was made possible when Sister Kate Anderson vacated her residential suite on the ward 23 corridor. The report noted that ” Ward 21, which has for some years been used to accommodate the patients from the artificial kidney unit will now be able to revert to its proper function as a metabolic ward.” The suite of rooms was designed in collaboration with Dr John Bowie, the hospital bacteriologist, to protect against infection. These rooms were later to be used for a variety of procedures including that of housing patients with bone marrow transplants.
After 1962 dialysis for patients with ARF was carried out in the Renal Isolation Unit (RIU). There were 4 dialysis beds in 4 small ventilated rooms. To prevent cross-infection, reverse-barrier nursing was practised: there was positive pressure ventilation, designed to prevent air-borne spread of infection from one room to another, and the staff wore theatre gowns and masks. Staphylococcus was the main concern during the first year, and commensal organisms in subsequent years. Four Kolff-Travenol twin coil artificial kidneys were acquired. The Kolff bath would be made up in the original AKU room and the machine wheeled to the RIU. The 1962-63 RIE annual report stated that 46 new patients were admitted to the RIU for dialysis.
In the Renal Unit in Edinburgh, there was an emphasis on the importance of minimising cross-infection. Such a policy was not adopted in all the dialysis units in UK. In the late 1990s the unit was brought into use again, and subsequently used to isolate MRSA-positive patients from other dialysis outpatients.
| Document – Letter from the treasurer to the secretary regarding the isolation unit at RIE ward 23 to be named “the Isolation Unit” (from the Lothian Health Service Archive) Click here to view. |
Reaction to haemodialysis for patients with acute renal failure
The Scotsman reported the opening of the first artificial kidney unit in Edinburgh (May, 1959), but there was no further press coverage on haemodialysis for renal failure, so the public was not widely aware of it.
| “It was a very exciting time for all of us. The early patients were relatively young, and after dialysis they got better. These patients would have died without dialysis. There was a good team spirit among the doctors, who were all under 37 years old at the time! Collaboration with colleagues (physicians, surgeons, laboratory staff) was developed in a scale rarely attempted before.” (Dr A Lambie)
“Patients were very ill before dialysis, so the patients who were dialysed and their relatives were very grateful for this new form of treatment.” (Sister S Green) |
The Renal Unit in the 1960s, 1970s and 1980s
In the early days most of the patients treated were young. During the 1970s, the severity of illness of patients treated for acute renal failure increased. There was no intensive care unit (ITU) at this time, and ventilation and cardiovascular monitoring had to be undertaken in the Renal Unit, with help from anaesthetists. The work of the Renal Unit increased steadily from 65 dialyses on 50 patients with ARF between the years of 1959 and 1960, to more than 800 patients treated by 1981. However much of the pressure came from the increasing numbers of patients with chronic renal failure coming forward for treatment, which put substantial pressures on the personal and financial resources of the Unit. Read more about dialysis for chronic renal failure and the later history of the Unit.