Contents
Screening for diabetes
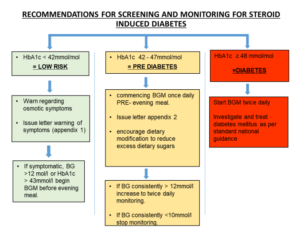
New onset diabetes after transplantation (NODAT) is observed in 10-20% of transplant recipients at 5 years. Risk factors include steroids, CNIs and sirolimus, previously impaired glucose tolerance, obesity and family history of diabetes. Steroid induced diabetes is defined as >2 occasions of a capillary blood glucose >12mmol/L in 24 hours. An HbA1c >48 is diagnostic of diabetes.
An HbA1c should be checked on admission for all potential kidney transplant recipients to guide risk assessment of developing NODAT, as outlined below:
Taken from: Lothian+Steroid+Safety+Bundle+approved.pdf (squarespace.com)
Risk should be assessed in all hospitalised patients on newly started or increased dose of steroids. Those individuals should have twice daily blood glucose monitoring regardless of diabetes status. If capillary blood glucose is >12mmol/L before the evening meal blood sugars should be checked 4 times a day.
Following discharge, newly transplanted patients should be screened for NODAT with a random glucose and HbA1c in the transplant clinic at the following time points:
- Weekly for the first month [Random glucose only]
- Monthly for months 2-6 [Glucose and HbA1c each time point here on]
- 3 monthly from 6 months to 2 years
- 6 monthly from 3-5 years
- Annually thereafter
Screening coincides with BK screening after the first month.
Patients starting steroids should be provided with an information sheet outlining the risk of diabetes and symptoms of hyperglycaemia e.g. Long term steroid use – patient information (2023)
Management of NODAT
A diagnosis of NODAT is confirmed with either a diagnostic fasting blood sugar (>7 mmol/L), >2 capillary blood glucose >12mmol/L in 24 hours, or an HbA1c >48mmol/mol.
Management is stepwise to achieve glycaemic control:
- Dietary advice
- Initiate gliclazide – institute home glucose monitoring via diabetes specialist nurses
- Refer to diabetes team for initiation of insulin if required.
The diabetes nurses can be contacted at: diabetesclinic.rie@nhslothian.scot.nhs.uk or on extension 21044.
The usual pattern of capillary blood glucose in steroid induced diabetes is a lower glucose at breakfast that increases throughout the day and falls overnight. This means that treatment is usually given in the morning and treatment at night should be cautious.
Immunosuppression should be reviewed with consideration given to:
- Early steroid dose reduction ahead of protocol
- Withdrawal of steroid
- CNI/sirolimus dose reduction
Steroid withdrawal or avoidance – edren.org
These decisions should be made on an individual basis with a full assessment of risk of rejection.
Patients with diet-controlled type 2 diabetes starting steroids post-transplant
Guidance on the management of patients on steroids and with type 2 diabetes not on insulin is available on the RightDecisions app under NHS Lothian diabetes: Steroids and diabetes.
- Consider starting treatment if blood glucose >12mmol/L for 3 days
- Start gliclazide 40mg OD; if blood glucose >20mmol/L insulin may be required
- Titrate dose in increments of 40mg daily to a maximum of 240mg (caution if eGFR<30 due to risk of hypoglycaemia)
- If blood glucose remains >12mmol/L for 3 days or >20mmol/L on one or more occasions then refer to diabetes for insulin start
- The DSNs should be contacted regarding patients who have required treatment for steroid induced hyperglycaemia as soon as discharge date is known.
Taken from: Lothian+Steroid+Safety+Bundle+approved.pdf (squarespace.com)
Patients on insulin starting steroids post-transplant
Guidance on the management of patients on steroids and insulin is available on the RightDecisions app under NHS Lothian diabetes: Steroids and diabetes.
If capillary blood glucose is above the target range suggested alterations to insulin are:
Once daily insulin: mixture insulin e.g. Humulin M3 or long acting insulin as monotherapy
- Give insulin in the morning and increase by 10-20% a day to meet targets
- Novorapid may need to be added with meals; avoid giving Novorapid at the same time as Humulin M3 due to the risk of hypoglycaemia.
Twice daily mixture insulin e.g. Humulin M3
- Increase morning insulin by 10-20% a day to meet targets
- Novorapid may need to be added at lunch; avoid giving Novorapid at the same time as Humulin M3 due to the risk of hypoglycaemia.
Basal bolus insulin
- Give basal insulin in the morning
- Increase Novorapid by 20% at breakfast and lunch
De-escalating steroid use in patients with diabetes
Steroid reduction and diabetes treatment de-escalation
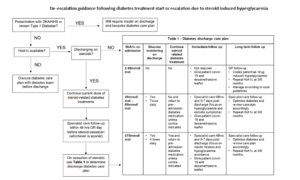
When steroids are reduced or stopped blood glucose levels fall. For patients stopping steroids completely there is a risk of sudden severe hypoglycaemia, and stopping steroid-related diabetes medications on cessation of prednisolone is recommended unless there was pre-existing suboptimal glycaemic control (HbA1c ≥70mmol/mol).
If diabetes treatment has been started/substantially escalated due to steroids, a plan must be made for de-escalation and the patient must be made aware of the risk of hypoglycaemia and be able to treat this.
Patients should be provided with:
- ‘Having a hypo’ guidance by Diabetes UK: https://www.diabetes.org.uk/guide-to-diabetes/complications/hypos/having-a-hypo
- Diabetes team contact details
De-escalation of treatment on discharge requires clinical judgement but the below is a guide:
Steroid withdrawal and risk of adrenal insufficiency
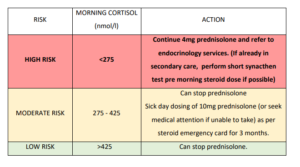
The risk of adrenal insufficiency when withdrawing steroids can be stratified by a morning cortisol sample taken prior to the steroid dose, once the prednisolone dose reaches 4mg or less:
Taken from: Lothian+Steroid+Safety+Bundle+approved.pdf (squarespace.com)