 What is IgA nephropathy?
What is IgA nephropathy?
IgA nephropathy (IgAN, also known as Berger’s disease) is a kidney disease, which affects the glomerulus. Glomeruli are the tiny blood filters where urine is made. IgA nephropathy is the commonest “glomerulonephritis” (inflammation of the glomerulus) found in the developed countries of the world. IgA is short for immunoglobulin A, an antibody which usually helps the body to fight infections and toxins (poisons) encountered in the gut and the lungs. In IgA nephropathy, IgA is deposited in the glomerulus and sometimes goes on to cause problems. Although much research is trying to fnd out why, it is still not understood why IgA is deposited in the kidneys and why it only sometimes goes on to cause problems.
 |
 |
 |
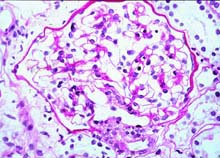
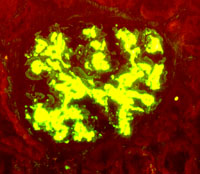
| Green fluorescence showing IgA deposited in the mesangium (middle part) of the glomerulus | Diagram showing the area of the glomerulus that IgA is deposited |
Is it serious?
In about one third of cases IgAN goes on to cause progressive damage to the kidneys (see Chronic renal failure and its progression) and some of these patients may need dialysis and/or transplantation in the end (see Dialysis and end-stage renal failure). IgAN tends to be very slowly progressive and so the process of the kidneys failing can take 10 to 30 years. At the time of diagnosis, it is often possible to tell whether there is a high chance of your kidneys becoming damaged with time or whether your outlook is good.
 What are the symptoms of IgA nephropathy?
What are the symptoms of IgA nephropathy?
- Most commonly there are no symptoms at all. The urine of patients with IgAN usually contains a small amount of blood, sometimes with protein. In most cases this is such a small amount of blood that it can not be seen (“microscopic haematuria“) and it can only be detected by putting a special dipstick into the urine. The most frequent way of this condition coming to medical attention is by chance screening, e.g. urine screening at a work or at a GP medical examination.
- Some people will actually be able to see blood in their urine (“macroscopic haematuria”). Typically this happens in young people when they have a sore throat or chest infection. The urine usually turns dark brown and patients may notice discomfort over their kidneys (the upper part of the back, below the ribs), which settles as the urine clears. Occasionally these episodes may be triggered by other things like heavy exercise or gastroenteritis.
- Very rarely there is heavy loss of protein from the kidney, enough to cause fluid retention and swelling of the ankles. This is called the “nephrotic syndrome“, but it happens less often in IgAN than in many other forms of glomerulonephritis.
- High blood pressure may also be the first sign of IgA nephropathy.
 How is the diagnosis made?
How is the diagnosis made?
In about half of all patients the levels of IgA in the blood are raised and this, or a history of passing blood in the urine at the same time as an infection is suggestive of the diagnosis. However the only way to diagnose IgAN with certainty is for the patient to have a renal biopsy, (a tiny sample of one kidney is taken) and the kidney tissue is then examined under the microscope. Special stains are used to show that IgA is present. At the same time the whole sample is examined to see if there is significant damage to the kidney, which may help to predict the risk of future kidney problems.
 Can IgA nephropathy be treated?
Can IgA nephropathy be treated?
We have split this into treatments to alter the disease process and treatments to prevent or cope with the damage caused by the condition.
Altering the disease
A large number of treatments have been tried all over the world, but it is still not clear whether drugs and other treatments are helpful. In general this usually means that no treatment is particularly useful. Among the treatments which have been tried are :
Fish oil : may have an effect in reducing inflammation and scarring in the kidney when given to patients who have evidence of damage to their kidneys, although on balance, it probably does not make as much difference as first thought. The same effect could be achieved by eating very large quantities of oily fish. Because the quantities are so large, the oil is given as capsules. One advantage of fish oil is that it does not have the same risks as other treatments which damp down the immune system. However, some people find that fish oil is not that pleasant to take.
Steroids and other treatments to suppress the immune system : Because IgA is part of the immune system some people believe that damping down the immune system with “immunosuppressant drugs” should help. Examples of immunosuppressants are steroids (such as prednisolone), cyclophosphamide, and cyclosporin. A number of these drugs have been tried on their own and in combination, but there is little evidence of definite benefit so far. It is important to remember that IgAN is a mild disease for most patients and that immunosuppressants have powerful and potentially serious side effects. Because they damp down the immune system they make the patient more vulnerable to infections, which may be serious. In addition steroids causes weight gain and may cause diabetes, they make the bones thin and more likely to break and tend to make the blood pressure go up. Many of the other immunosuppressants increase the risk of cancer. Because of these side-effects and the lack of evidence that they work, most British doctors feel that the risks are not justified in most cases of IgAN.
There are two exceptions when immunosuppressants may be considered:
- In patients whose kidney function is deteriorating rapidly and whose biopsy shows signs of a lot of inflammation
- If you have a lot of protein in your urine (nephrotic syndrome) a course of immunosuppressant treatment may sometimes be considered as they may help to protect the kidney function. However this is not yet proven. More information about immunosuppressant drugs and the kidney is available.
Diet : There are no foods known to cause IgAN, (though drinking excessive alcohol can cause a similar picture – if you think this may be the case you should tell your doctor). Similarly making changes to your diet will not change the underlying problem. If you have high blood pressure, you should avoid excessive amounts of salt, as salt tends to put up the blood pressure.
Antibiotics : Because macroscopic haematuria tends to come at the time of an infection, doctors used to think that treating or preventing infection may help prevent IgAN. Unfortunately a trial of a one year course of an antibiotic didn’t have any effect on the amount of protein lost in the urine or on the degree of damage to the kidneys. There was a reduction in the amount of haematuria. There is therefore no advantage to taking antibiotics, unless the provoking infection is bad and needs treatment in its own right.
Tonsillectomy : Again, taking out the tonsils reduces haematuria if tonsillitis is the provoking infection, but it does not affect the long term kidney function. There is no convincing evidence that tonsillectomy prevents IgA nephropathy or renal failure.
 Preventing and coping with kidney damage from IgA nephropathy
Preventing and coping with kidney damage from IgA nephropathy
High blood pressure : (“hypertension”) is the commonest and most important consequence of IgAN. Treatment of high blood pressure is essential because:
| High blood pressure can cause heart disease and stroke |
| High blood pressure worsens kidney damage in people with kidney diseases. |
In kidney disease, blood pressure control is therefore very important it can prevent kidney failure.
There are theoretical reasons why some blood pressure treatments (“ACE inhibitors”) may be better than others if you lose protein in your urine. ACE inhibitors tend to reduce the amount of protein lost and protect the kidneys. More information on blood pressure and the kidney.
Chronic renal failure:
Other aspects of treatment of chronic renal damage are described in our page on chronic renal failure and its progression.
Dialysis and transplantation : in a small minority of patients the kidneys fail completely (“end-stage renal failure”) and they need dialysis treatment to keep them well. If this happens all patients will be considered for kidney transplantation : and most go onto the waiting list. In general, patients with IgAN do well with transplantation, but there is some evidence that after time IgA may be deposited in the transplant kidney causing IgAN to recur. Even if it does, it usually takes ten to twenty years before the kidney fails completely.
 How can I find more about it?
How can I find more about it?
The Canadian IgA Nephropathy Support Group has created a carefully edited and balanced set of pages about IgA nephropathy, and has online discussion groups and other resources for patients. Recommended. There is a lot of information about IgA disease on the Internet, but some is not completely reliable.
Other sites of interest : The following EdREN Info pages are relevant:
Acknowledgements: The author of this page was Dr K Buck. It was first published in November 2000. The date is was last modified is shown in the footer.
