This is a late microvascular complication of diabetes mellitus which typically appears after more than 20 years of type I diabetes. Most patients with diabetic nephropathy already have diabetic retinopathy, and many also have evidence of neuropathy. In type II diabetes it is common for subclinical diabetes to have been present for many years, so that complications may be identified at the time of diagnosis.
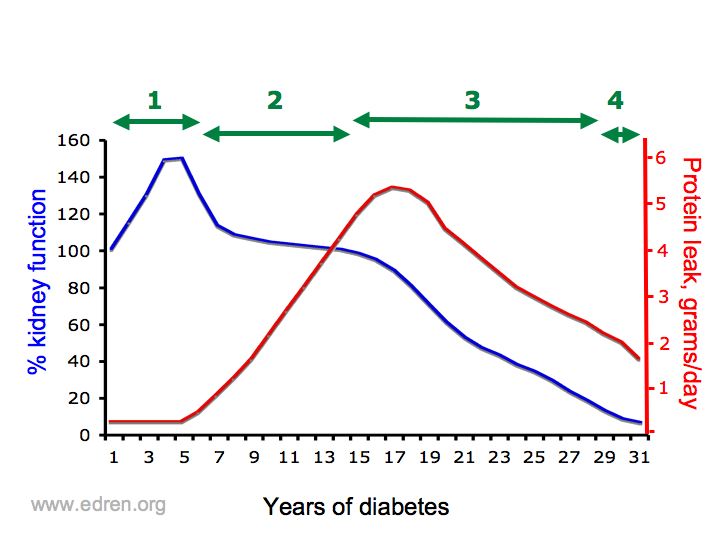
Patients move through characteristic phases:
- Hyperfiltration – elevated GFR (Phase 1 in diagram)
- Hypertension (still 1)
- Microalbuminuria, identified by sensitive immunoassays for albumin (dipstick tests for protein remain negative but albumin excretion >20mg/mmol creatinine) (still 1)
- Overt proteinuria (dipstick tests positive) = overt diabetic nephropathy (2)
- Nephrotic syndrome (2/3 junction)
- Progressive renal impairment. If unmodified by treatment, this can lead to ESRF over 1-2 years (3-4)
Contents
Risk factors
Not everyone gets diabetic nephropathy – about a third of patients do eventually, but there are risk factors
- Poor diabetic control
- Duration of diabetes
- Presence of retinopathy and other microvascular complications
- Race – some races have a markedly higher incidence of nephropathy
- Family history – perhaps segregating with susceptibility to hypertension and other renal diseases
Diagnosis
Other types of renal disease can occur in diabetes, but in the presence of other complications and with the characteristic progression, the etiology can usually be safely assumed. If there are atypical features then renal biopsy may be considered.
Preventing development and progression of diabetic nephropathy
Controlled trials have shown unequivocally that diabetic nephropathy can be prevented, or its progression arrested, at stages at least up to the development of abnormal renal function. Sometimes even abnormal renal function can be protected.
- Control of blood sugar reduces the risk of developing proteinuria, and stringent control can reverse microalbuminuria before overt proteinuria has developed.
- Blood pressure control reduces the rate of loss of renal function. More on hypertension.
- ACE inhibitors and ARBs reduce and in some instances abolish proteinuria. In individuals in whom proteinuria is reduced, the rate of loss of renal function is reduced, or abolished. This effect is not restricted to patients with hypertension, and exceeds the effect of blood pressure control alone. Hyperkalaemia may limit use in patients with renal impairment. Diabetics are also at increased risk of ACE inhibitor-induced deterioration of renal function in the presence of renal artery stenosis. More on ACE inhibitors
- Diet – the controversial role of protein restriction in controlling the progression of chronic renal failure is mentioned in the section on CRF.
Renal replacement therapy in diabetes mellitus
The mortality of diabetics with ESRF is substantially higher than averages for other patients with ESRF, particularly because of the high incidence of other diabetic complications, notably accelerated atherosclerosis. Difficulties with fluid balance, and gastrointestinal symptoms aggravated by autonomic neuropathy, commonly lead to earlier institution of dialysis in diabetics than in other patients.
Systemic diseases such as diabetes were once considered to be contraindications to renal replacement therapies. Diabetics with many complications may still have a difficult time on dialysis, because of ischaemic limbs, ischaemic heart disease, or autonomic neuropathy, or a combination of these.
Renal transplantation leads to a much greater improvement in quality of life. The perioperative risk of transplantation is higher than for other patients, but in the medium and longer term, improved survival in transplant recipients outweighs the perioperative risks in patients considered fit for transplantation. Transplantation is not considered as an option in many type II diabetics with ESRF because of the risks associated with vascular disease and relatively short prognosis for many patients.
Pancreatic transplantation carries additional risks, but also additional long term survival benefits. Many now regard combined kidney and pancreas transplantation as the treatment of choice in young type I diabetics with ESRF, although some are still excluded because of excessive risk.
Further info
Diabetic nephropathy – info for patients (edren/info)
Glomerulonephritis (edren textbook)