BK and JC are two polyoma viruses that are not associated with symptomatic infection in immunocompetent individuals, but are commonly acquired and lie dormant. They may cause significant disease in immunosuppressed patients. JC virus has only very rarely been reported to cause renal disease, and the brain disease that it can cause is extremely rare in renal patients. Kidney infection by BK virus is a well recognised problem though. Published evidence of BK nephropathy is almost completely limited to renal transplantation.
BK virus (BKV) infects more than 80% of individuals by early childhood, and persists in epithelium of kidney, ureters and bladder. Viruria is common following renal transplantation, and testing for this is not helpful. Viraemia is less common, and sometimes (not always) associated with nephritis.
BKV associated nephropathy (BKVAN) is a tubulointerstitial nephritis that has often been mistaken for rejection, and carries a high risk of graft failure. There generally are no extra-renal symptoms, signs, or test characteristics to suggest viral infection. The risk of BKVAN is highest in the first year after transplant, but is raised for up to 5 years. Occasionally it occurs later.
Contents
Screening and diagnosis
BKVAN is almost always associated with significant viraemia, making screening by PCR of blood potentially useful. Our protocol is to screen:
- First year after renal transplantation: Monthly for 6 months, at 1, 2, 3, 4, 5, and 6 months, then 3 monthly, at 9 and 12 months.
- Thereafter, every 3 months in year 2, and every 6 months in years 3-5, to a total of 5 years of surveillance.
- The laboratory will not process a request if <4 weeks has elapsed since the previous result (unless that sample had a positive result).
- In the event of a first positive result, a follow up test in <4 weeks (but not < than 2 weeks) is warranted. In this instance, it should be specified on the clinical information that this is a follow up of a positive result to ensure the request is processed.
Diagnosis of BKVAN usually requires a renal biopsy. Some centres use urine cytology to identify virally infected cells. Infected cells can be identified microscopically, but immunostaining for polyoma antigens is much more sensitive.
A biopsy may not be necessary if:
- Viral load is low, or falling, AND
- Allograft function is stable
Management: reduction of immunosuppression
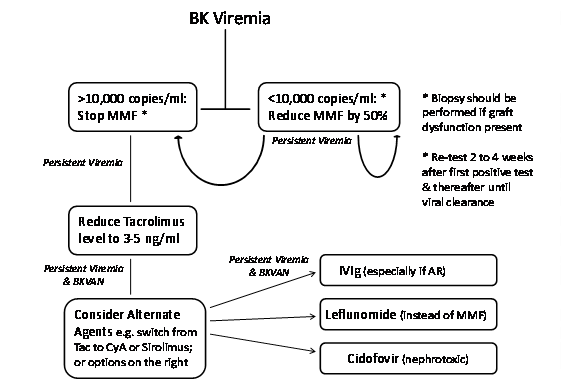
Reduction in immunosuppression is the cornerstone of BKV management. However there is no clear consensus on the viral load above which therapy should be altered. 10,000 copies/ ml is a possible reference point, but as assays are generally not standardised, this can only be considered a rough guide.
The most robust data supports initially reducing or stoppping the antimetabolite (generally MMF), with later reductions in tacrolimus if viraemia or nephropathy persists. Other options include switching tacrolimus for cyclosporine or even sirolimus.
- Corticosteroids are generally continued at the same dose, as other agents are reduced
- Renal function and BKV levels should be monitored 2-4 weekly
- Check Donor Specific Antibodies (DSA) if the anti-metabolite is stopped for more than 4 weeks
After viral clearance – many practitioners see BK viraemia as a sign of over-immunosuppression and do not routinely return to previous dose of anti-metabolite. It may be necessary to balance this with perceived immunological risk, monitoring viral load.
This protocol has been used in Edinburgh, though use of alternative therapies is now rare (see below):
Alternative agents for BKVAN
These are all unproven and generally not indicated.
- IVIG – contain anti-BKV neutralising antibodies, but there is no robust evidence that it alters the course of nephritis.
- Leflunomide – has both immunosuppressive and antiviral activity. The therapeutic dose is uncertain and liver and bone marrow toxicity may occur. There are other significant side effects. There is no good evidence from clinical studies to support its use.
- Cidofovir – has modest in vitro antiviral activity agains BKV, but is itself nephrotoxic. Currently there is only very weak justification for using it or related compounds.
Concomitant BKVAN and acute rejection
Difficult to be sure of, as histological appearances cannot easily distinguish the unless the rejection is antibody-mediated, in which case IVIG has been used.
Retransplantation
Retransplantation after graft loss from BKVAN has generally been successful. Be sure viraemia is cleared.
Further info
- Info for patients about BKV (Edren)
Page by [?], modified from a 2015 appendix. Last modified date shown in footer.