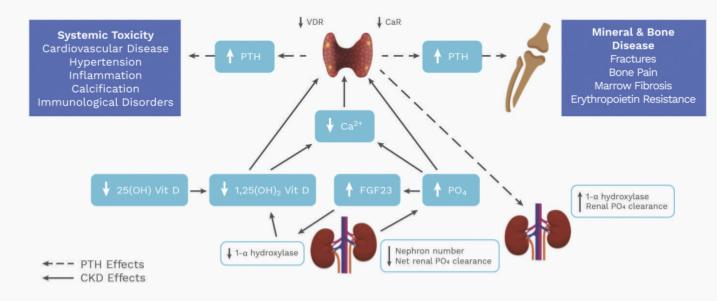
Calcium and phosphate homeostatis is altered in advanced CKD and secondary hyperparathyroidism is common in our dialysis population. Below is a brief infographic summary from the 2017 KDIGO clinical guidelies. For our full education page on osteodystrophy, click here.
Management of CKD-MBD is focussed controlling hyperphosphataemia and maintaining serum calcium levels within the normal range. This is achieved through a combination of dietary restriction of phosphate, prescription of phosphate binders and calcimimetics, and – in some patients – parathyroidectomy.
Monitoring frequency of phosphate, calcium and PTH levels will depend upon the presence and magnitude of abnormalities, and the rate of progression of CKD. For haemodialysis patients in NHS Lothian and Borders, phosphate and calcium are checked every 4 weeks, and PTH every 3 months.
For patients with CKD and those post-transplantation, monitoring is usually undertaken less frequently. As the optimal PTH target has not been established for patients with CKD who are not on dialysis, the remainder of this page will refer to those on dialysis.
Calcium and PTH
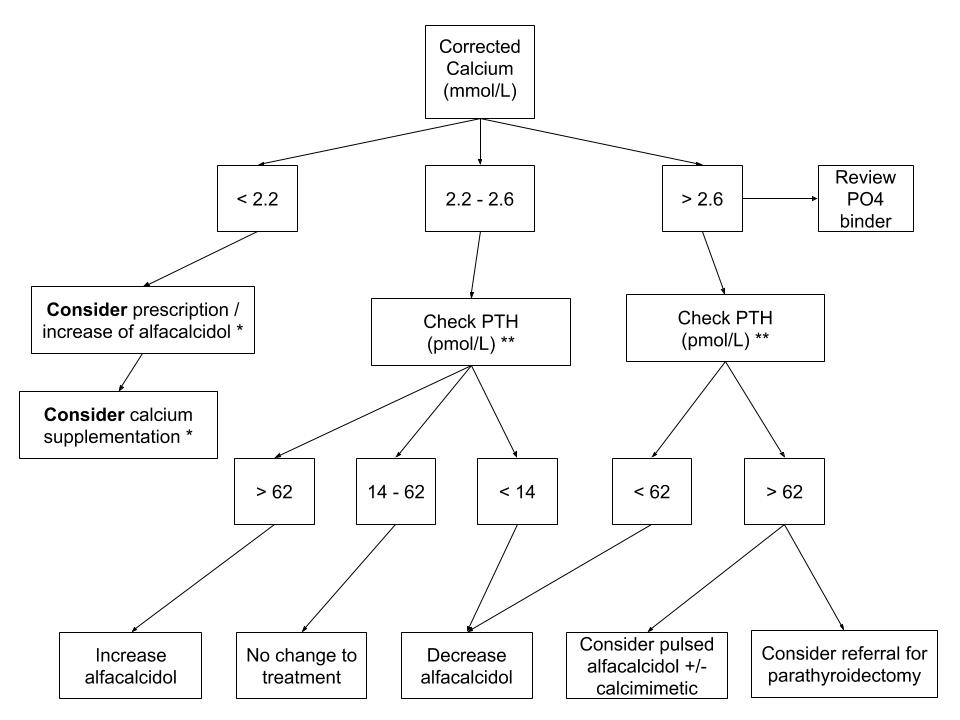
Total calcium should be measured every 4 weeks and is corrected by adding 0.02 for every g/L the serum albumin is below 40g/L. This adjusted calcium measurement can be used, along with PTH, to determine treatment according to the calcium algorithm below:
* Treatment of hypocalcaemia should be individualised. Mild and asymptomatic hypocalcaemia may be tolerated in order to avoid a positive calcium balance.
** Modest increases in PTH levels may represent an appropriate adaptive response to decreasing kidney function. Therefore, the target range for PTH levels in hyperparathyroidism is usually higher than the normal range in order to prevent adynamic bone disease, and treatment recommended based upon trends in PTH level rather than a single elevated value.
In NHS Lothian at present, PTH is measured in pmol/L, with the upper limit of normal being 6.9pmol/L. The guidance in the algorithm above is calculated using this parameter in accordance with KDIGO guidelines, which recommend a target PTH of between 2 and 9 times the upper limit of normal (i.e. between 13.8 and 62.1 pmol/L).
Phosphate
Phosphate is measured every 4 weeks in haemodialysis patients to adjust therapy with phosphate binders. This can be done using the phosphate algorithm below. Regular dietician review is crucial in enabling patients to achieve adequate phosphate control. 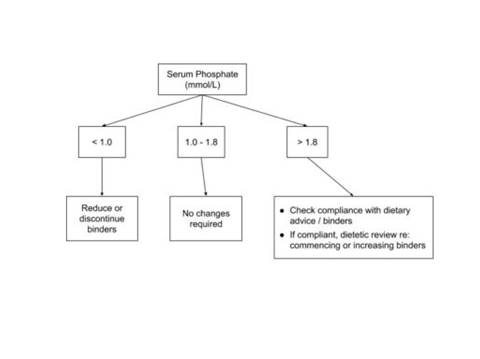
Phosphate binder type and dose is decided using measurements of corrected calcium and phosphate. Click here to view the most recent phosphate binder treatment ladder.
Parathyroidectomy
Patients are at risk of profound hypocalaemia immediately after parathyroidectomy (and then at risk of hypo- or hyper-calcaemia if vitamin D and calcium supplements are not titrated appropriately in the following weeks). Close monitoring and pro-active vitamin D / calcium supplementation is vital.
See our unit protocol for care of CKD patients undergoing parathyroidectomy.
References
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic
Kidney Disease–Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2017;7:1–59.
Acknowledgements: Neil Turner was the main author for this page. It was updated by Ashley Simpson in September 2020. Eoin O’Sullivan added an updated parathyroidectomy protocol in July 2021.