You are the FY1 on a busy medical take. You are asked to see a gentleman who presented to his GP following a few days history of general malaise, back pain and decreasing urine output. He has not passed urine today.
Image from istocks
You are able to access the blood tests which show the following results:
Hb 120, WCC 11.0, Neut 5.3, Plt 273
Creat 684 (82), Urea 10.0, Na 140, K 5.5
What first steps do you need to undertake?
Whilst there is a significant deterioration in his renal function, it is not currently at a level where you might expect this gentleman to require dialysis. You need to gather a bit more information about his presentation
This would be one of the most important first steps. You would need to ask:
- History of condition- including any recent illness, new symptoms, urinary issues including visible haematuria, recent instrumenting of urethra or bladder
- Past medical history – any previous bladder issues or prostate issues
- Medications – any new
- Family history of any renal issues
- Systematic review
- Patient concerns
Whilst this may form part of investigations, there are other more pressing things that need to be done in terms of learning what is going on in this gentleman’s case
This is an important part of initial workup. This would include
- Any signs of sepsis – fever, tachycardia, hypotension
- Abdominal examination – localise pain – ? back/ ? flank, Palpable bladder?
- Fluid balance – oedema – facial, sacral, peripheral; JVP;
- Any signs of cardiovascular or liver impairment
This is a simple investigation which can be used to rule out urinary retention.
You undertake the above salient investigations
Click Reveal to show the answer
The patient describes a history of sometimes seeing dark urine over the past 6 months with gradually smaller amounts being passed in the last few days. He has not passed any urine in the last 24 hours. He has not recently been unwell but has had some difficulty at times starting to pass urine. He is not taking any medication. He has no family history of renal conditions. He has noticed that his weight has increased and that he has leg swelling
Examination revealed he patient is sitting upright with a respiratory rate of 35 breaths per minute. Blood pressure is 168/100, heart rate 105 regular. His neck veins are visible and his JVP is elevated at 6cm. His heart sounds are normal but respiratory examination demonstrates bibasal dullness and basal fine crepitations. He has pitting oedema to his mid-thighs.
Bladder scan shows 50mls of urine in his bladder
What would be your next action in this gentleman’s presentation
Yes this is an important aspect of further work up for this gentleman. It will show up any abnormalities anywhere in the renal tract and point towards a possible diagnosis. Ultrasound is the usual first imaging modality
Whilst this would seem a good treatment choice and may be of benefit once the patient is stabilised, these will only be of benefit if he is producing urine.
This may be useful in determining if the dark urine is just concentrated or if there are large volumes of protein or blood in the urine. Note it is not useful in ruling out or in infection and for that urine culture and clinical correlation with signs and symptoms is most appropriate.
This gentleman has signs of pulmonary oedema and peripheral oedema. As such carefully managing his fluid balance to assure he is not drinking too much as to continue to accumulated fluid would be an important step in his management.
Write down what you think the most likely diagnosis for this gentleman is?
He undergoes ultrasound scan of his renal tract. Click reveal to find out what this showed.
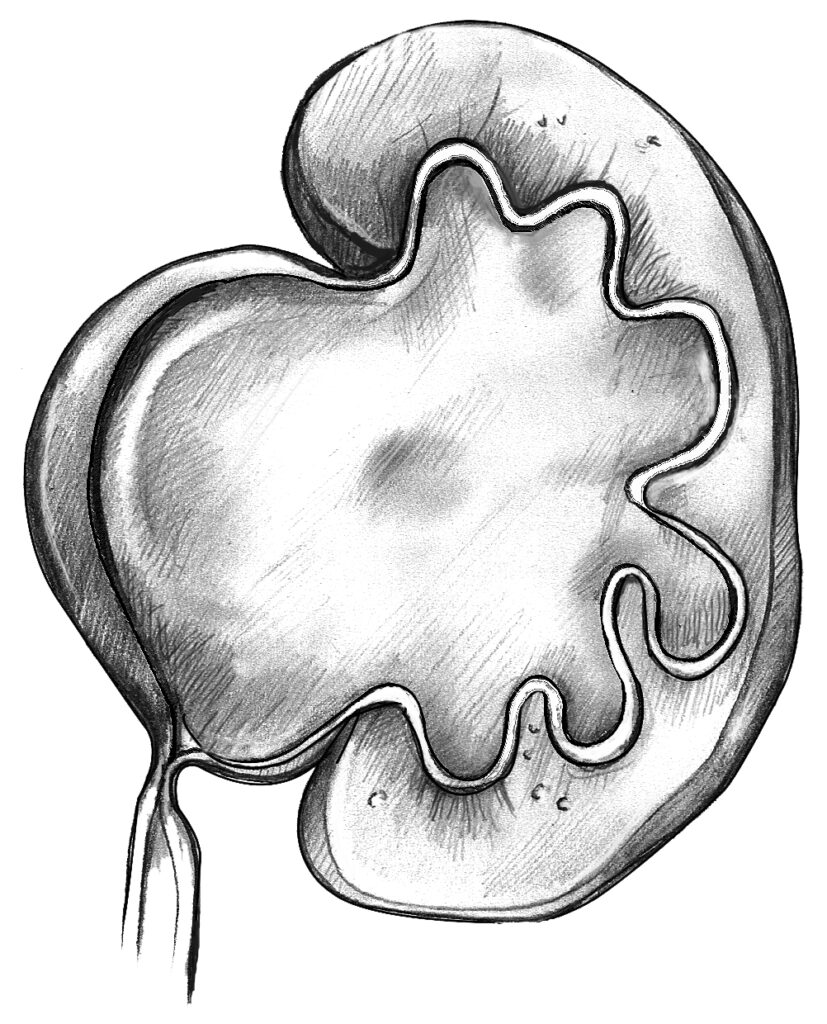
“The left kidney is 10.5 cm in length with gross hydronephrosis and dilation of the collecting system. The cortex is of normal thickness. The right kidney is 7.5 cm in length with dilation of the ureters and collecting system. There is a loss of cortical thickened throughout. The bladder is empty with evidence of a thickened wall posteriorly”.
Given these results what treatment would you suggest
The right kidney is atrophied and effectively dead. Placing a nephrostomy tube in the right kidney is unlikely to help.
Whilst this may come as follow-up, it is not appropriate just now. The main aim is to optimise this gentleman’s kidney function. CT scan may also introduce contrast which would not be appropriate given his current renal function.
This would be the most appropriate option to improve his renal function. This should be undertaken urgently in an attempt to improve long-term kidney function.
A urogram will be of little value in an obstructed kidney as the contrast will only be taken up very slowly and the images will be very poor. In addition contrast will be needed which will act as a further renal insult.
The appropriate action is taken and his renal function slowly starts to improve. He is listed for a ureteric stent and further investigation as to why this obstruction occurred. Follow-up with the renal team is arranged as his renal function does not return to normal.
You have now completed the case.
