Contents
Renin-Angiotensin Aldosterone System (RAAS) Blockade
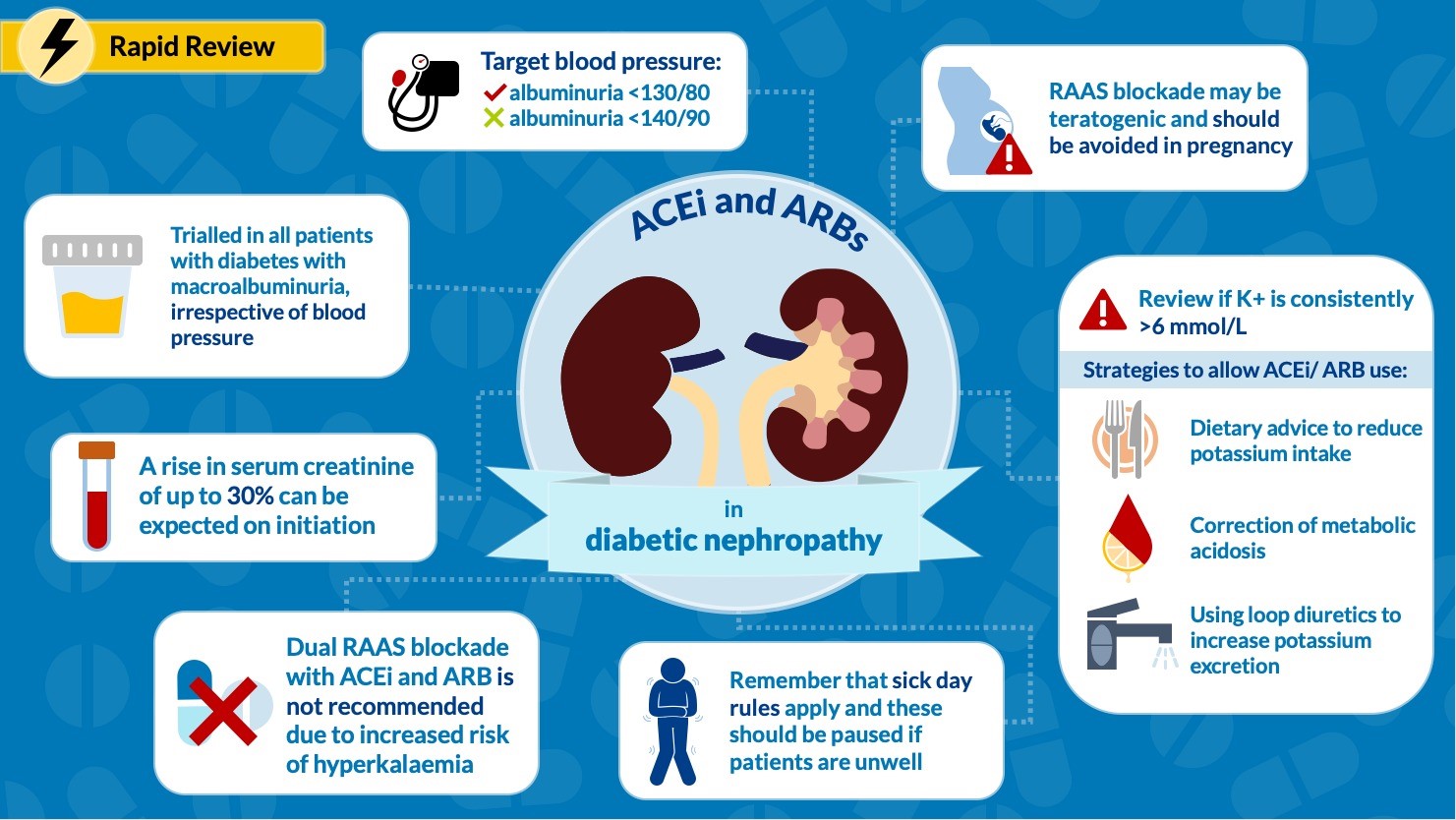
ACEI/ARB therapy should be considered for most adults with diabetes and persistent micro- or macroalbuminuria, irrespective of blood pressure. The dose of ACEI/ARB should be titrated to the maximum tolerated. Dual RAAS blockade is not recommended due to risk of hyperkalaemia and AKI. RAAS blockade in patients with diabetes who are normotensive and normoalbuminuric is not recommended. A rise in serum creatinine of up to 30% can be expected on initiation of ACRI/ARB therapy.
Blood pressure targets (as per KDIGO guidlines):
- Target <130/80 mmHg in the presence of albuminuria
- Target <140/90 mmHg if no/low albuminuria
It would seem reasonable to suggest a target systolic blood pressure of no less than 150 mmHg in much older patients with CKD, taking into account side effects of medications and comorbidities.
Given the potentially teratogenic nature of RAAS blockade drugs, the use of these drugs in women of childbearing age should be balanced with the risk of pregnancy. RAAS-blocking drugs should be stopped when pregnancy is planned / confirmed.
RAAS blockade should be reviewed if serum potassium is consistently >6mmol/L and other drugs known to promote hyperkalaemia have been discontinued. The Renal Association suggests dietary advice, correction of acidosis and loop diuretic therapy to lower serum potassium as necessary in patients with diabetes and CKD stages 4 and 5 for safe use of an ACEI/ARB. In the presence of hyperkalaemia, where bicarbonate is less than 22 mmol/l, sodium bicarbonate can be added at a dose of 500 mg twice daily: larger doses can be used but often require a concomitant increase or addition of a loop diuretic dose due to associated fluid retention.
For blood pressure control or fluid balance management, It may be reasonable to consider adding in an aldosterone antagonist, such as spironolactone or eplerenone, particularly for patients with an eGFR of greater than 60 ml/min/1.73m2 and a serum potassium of less than 5 mmol on a maximal dose of ACEI or ARB.
During an acute illness, particularly when a patient has volume depletion, there is a risk that patients with diabetes and CKD stages 4 and 5 who are taking an ACEI / ARB will develop AKI. Such risk can be avoided by stopping the ACEI / ARB treatment for the duration of the illness and for 24–48 hours post recovery.
Calcium Channel Blockers
Non-dihydropyridine calcium channel blockers (e.g. diltiazem and veraparmil) have been shown to reduce proteinuria in diabetic kidney disease. These can be used as an adjunctive therapy for patients with diabetic kidney disease who are persistently proteinuric despite maximal RAAS blockade, or as an alternative treatment when patients are intolerant of RAAS blockade. Non-dihydropyridine calcium channel blockers have been shown to decrease proteinuria greater than dihydropyridine calcium channel blockers (e.g. amlodipine and nifedipine).
Sodium Glucose Cotransporter 2 (SGLT-2) Inhibitors
Sodium glucose cotransporter-2 (SGLT-2) inhibitors (e.g. canagliflozin, dapagliflozin and empagliflozin) offer the possibility of renal protection in diabetic kidney disease independent of their glucose-lowering effects. SGLT-2 inhibitors have been shown to reduce progression of diabetic kidney disease, and their use is associated with a relative reduction in risk of death from end-stage renal failure and cardiovascular events (2,3). See our guidance on prescribing SLGT-2 inhibitors.
Finerenone
Finerenone (a non-steroidal MR antagonist) may be considered as an add-on therapy in patients who have albuminuria despite optimal RAAS blockade and SGLT2 inhibition. See our protocol in the pharmacy handbook.
References
1. https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-Blood-Pressure-Guideline-English.pdf
2. Perkovic V et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy.N Engl J Med. 2019 Apr 14. doi: 10.1056/NEJMoa1811744
3. Ingelfinger JR, Rosen CJ. Clinical Credence – SGLT2 Inhibitors, Diabetes, and Chronic Kidney Disease. N Engl J Med. 2019 Apr 14. doi: 10.1056/NEJMe1904740.
Acknowledgements: Ashley Simpson was the main author for this page. Infographic created by Michelle Lim. It was first published in November 2020. The last modified date is shown in the footer.