Contents
Acute kidney injury (AKI)
AKI is very common, occurring in up to 10% of all hospital admissions and it is usually identified on the basis of blood results or fluid balance charts first reviewed by a junior doctor…hence it is essential to be able to recognise and manage AKI.
AKI is a sudden deterioration of kidney function. Like most forms of kidney disease, it is often silent and only detected by a rise in serum creatinine or a fall in urine output. AKI can be graded based on severity:
1. Increase in serum creatinine by ≥26.5micromol/L within 48 hours or
2. Increase in serum creatinine to ≥1.5 times baseline within the prior seven days, or
3. Urine volume <0.5ml/kg/hr for ≥ six hours (e.g. <30ml/hr in a 60kg person)
Note that the eGFR will be misleadingly high in patients with AKI as the creatinine level on which this is based is rapidly increasing. As an extreme example, if a patient with a single functioning kidney undergoes nephrectomy, the serum creatinine might increase from 80 pre-op to 200μmol/L, the following day. With a creatinine of 200μmol/L, the eGFR will be reported as 24ml/min, however clearly the true eGFR is negligible! Hence, the best method of assessing renal function in AKI is the rate of change in creatinine.
In the absence of previous blood results, AKI rather than CKD may be suggested by the results of other investigations such as:
1. Normal kidney size on USS (chronic kidney disease often causes small, fibrosed kidneys)
2. Normal haemoglobin (the half-life of a red blood cell is 120 days, so if failed kidneys stop producing EPO it would take several weeks to become anaemic in the absence of other causes)
3. Normal PTH (hyperparathyroidism secondary to renal failure takes some time to develop)
If in doubt as to whether your are dealing with AKI or CKD, presume it is AKI and act quickly as:
- AKI may progress rapidly
- If treated quickly, it may be readily reversible
AKI may be classified for diagnostic and management purposes into (see figure):
- Pre-renal failure (see below) accounts for the majority in hospital
- Post-renal – i.e. obstruction accounts for a lot. See obstruction page
- Renal – intrinsic renal disease disease – glomerulonephritis and interstitial nephritis.
Pre-renal AKI and acute tubular necrosis
Pre-renal AKI is associated with reduced renal blood flow caused by hypotension due to:
1. Severe dehydration – poor oral intake, excessive GI, skin or urinary losses
2. Septic shock
3. Haemorrhagic shock
4. Cardiogenic shock
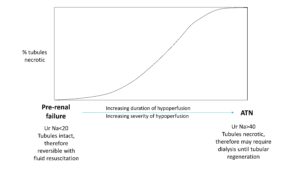
If the hypotension is transient or not severe, pre-renal AKI may be readily reversible by fluid resuscitation and treatment of the underlying cause. In pre-renal AKI, the tubules remain intact and will appropriately avidly retain salt and water to defend blood volume, hence it is characterised by low urinary sodium (typically <20mmol/L, due to activation of the renin-angiotensin-aldosterone system), and high urinary osmolality/specific gravity (due to secretion of ADH).
When hypotension is very severe or prolonged, acute tubular necrosis (ATN) may develop due to ischaemic injury, hence the need to treat low blood pressure promptly. Once the tubules are necrotic they no longer function appropriately to conserve salt and water and hence urinary sodium may be elevated (>40mmol/L) and the urine may be inappropriately dilute. Importantly, once ATN develops, fluid resuscitation alone is unlikely to improve kidney function as the kidneys will not recover until the tubules regenerate and this can take several days or weeks. Hence it is important to resuscitate aggressively and early, but once blood the clinical examination indicate the patient is euvolaemic, reduce fluid administration to match the urine output.
Mortality of over 50% for ATN occurring in hospital is usual, not just because of renal failure directly, but also because of its association with failure of other organs and with severe sepsis.
Intrinsic kidney disease
While this accounts for a minority of AKI, it is very important to recognise as it often needs specific treatment to recover renal function. It may be classified according to the compartment of the kidney affected:
Renal vasculature
Although sometimes considered as pre-renal failure, occlusion of the large vessels (aorta/renal arteries) or small vessels (haemolytic uraemic syndrome, malignant hypertension) is typically associated with high blood pressure and does not respond to fluid resuscitation, therefore is best considered within the spectrum of renal disease. Here the urinalysis typically shows no or minimal blood and protein
Glomerular disease
Glomerular diseases that may present with a rapidly progressive glomerulonephritis (RPGN) picture include: anti-GBM, small vessel vasculitis, post-infectious glomerulonephritis, infectious endocarditis and occasionally IgA nephropathy. Here the urinalysis typically shows blood and protein
Acute tubular necrosis
This is the most common cause of AKI in patients in ICU. In addition to being a consequence of prolonged ischaemic damage as described above, tubules may be damaged/blocked by toxins such as hypercalcaemia, myoglobin (rhabdomyolysis), light chains (myeloma), crystals (oxalate crystals in ethylene glycol poisoning) or drugs (aminoglycosides, cisplatin). Here the urinalysis typically shows no or minimal blood and protein
Acute interstitial nephritis
Unlike ATN, which is caused by ischaemic or toxic injury, interstitial nephritis is an idiosyncratic allergic response, typically to drugs such as antibiotics (penicillins, cephalosporins), NSAIDS or proton pump inhibitors. Here the urinalysis typically shows no or minimal blood and protein, but may be positive for leucocytes.
Post renal disease
Obstruction to flow in the renal tract may cause renal failure, but it needs to affect both kidneys (unless you have a single functioning kidney). For this reason, the obstruction is typically at the level of the bladder outlet, usually in older men due to benign prostatic hypertrophy. It is less likely that both ureters will be blocked simultaneously by stones, but they may both be obstructed by bladder tumours invading the lower ureters or external compression (e.g. aortic lymphadenopathy or retroperitoneal fibrosis.
The presence of complete anuria suggests a mechanical problem, such as obstruction or arterial thrombosis. However, obstruction can paradoxically present with polyuria when the back pressure causes tubular injury and a concentrating defect, while the obstruction is intermittent allowing some urine to pass.
Rarely a single cause
In practice, ATN and pre-renal failure short of ATN are usually associated with other risk factors such as sepsis, or exposure to predisposing or nephrotoxic drugs (notably NSAIDs, ACE inhibitors, diuretics; aminoglycoside antibiotics, vancomycin) or other toxins (e.g. myoglobin in rhabdomyolysis). It is more likely in the presence of pre-existing renal impairment, and in the elderly, and usually occurs in the context of other severe illnesses. Mortality of over 50% for ATN occurring in hospital is usual, not just because of renal failure directly, but also because of its association with failure of other organs and with severe sepsis.
Renal artery (or aortic) occlusion is true pre-renal failure, in the absence of signs of shock. There are usually other signs of vascular occlusion.
Approach to the patient with oliguria
1. Is the AKI real – check the U+E result is genuine or in those with anuria flush an indwelling catheter to check that it isn’t blocked
2. Could it be pre-renal failure?
- Assess circulatory state – capillary refill, blood pressure (versus patient’s normal, erect and supine BP may be informative to identify early volume depletion), JVP, mucous membranes
- Check fluid balance– input and output over last 48h or longer. Any extra losses – vomiting, diarrhoea, fever, drains, third spacing due to sepsis, abdominal surgery
- Check meds: new start/increase dose in diuretics, on ACE/ARB or NSAID that may exacerbate AKI?
- If suspicion of pre-renal, then fluid resuscitate and re-assess frequently. If no haemodynamic improvement once >2L challenge, seek advice of senior colleague
3. Could it be post-renal failure?
- Is the bladder palpable?
- Is person at high risk: male >60yrs, history of bladder/cervical cancer, visible haematuria, loin pain
- Do a bladder scan or order ultrasound scan of renal tracts
4. Could there by an intrinsic renal problem?
If there is no evidence of pre-renal and post renal problems, think renal causes:
Toxic ATN: drugs (e.g. aminoglycosides, cisplatin), myoglobin (check for dark urine if muscle pain), hypercalcaemia, myeloma casts (especially if anaemia/pancytopenia )
Tubulointerstitial nephritis: often due to drugs – penicillins, cephalosporins, NSAIDs, proton pump inhibitors, etc – check if eosinophil count raised, leucocytes on urinalysis in the absence of infection (but little blood/protein)
Glomerulonephritis – typically blood and protein on urinalysis. Consider post-infectious glomerulonephritis (check ASOT, complement), vasculitis (check CRP, ANCA if systemic symptoms), anti-GBM disease (especially if haemoptysis), IgA/Henoch Schloein Purpura (often with skin rash), occasionally lupus nephritis (check ANA/dsDNA)
Regardless of cause, optimise circulation (fluid replacement; ?inotropic agents), but carefully – over-hydrated patients with established AKI have significantly worse outcomes. Hence, resuscitate early, but perform regular fluid balance assessment and once euvolaemic simply replace urine output.
Important investigations in AKI
- Urinalysis – heavy proteinuria suggests glomerular disease. Haematuria may suggest glomerlonephritis if taken before catheterisation and in the absence of urine infection.
- Ultrasound – immediately diagnoses/excludes obstruction, identifies chronic scarring, missing kidneys etc.
- Chest X-ray – check for evidence of pulmonary oedema
- Cultures of blood, urine, any wounds or drains. Infection is very common as cause and complication.
- In more detail – including additional tests if intrinsic renal disease seems likely – Tests in acute renal failure (edren handbook)
Management of established AKI
- Control intake of fluid. If patient is euvolaemic on fluid balance, simply replace predicted losses (+ 500mls ‘insensible’ loss)
- Treat primary cause where possible
- Indications for dialysis or other renal replacement therapy:
- Pulmonary oedema
- Severe hyperkalaemia despite medical management
- Symptomatic, or very poor biochemical results, and unlikely to recover renal function quickly
- Pericarditis
Dialysis
Peritoneal dialysis is now rarely used in AKI. Haemodialysis may need to be given frequently (e.g. daily) in order to prevent large fluid swings and give enough biochemical clearance. Slow continuous treatments (haemodialysis or haemofiltration) are often used in an intensive care or high dependency setting. Prescribing dialysis in ARF from the EdRen Handbook
After AKI
A polyuric phase is typical in the recovery phase of ATN in previously healthy kidneys, but not universal. It is partly due to excess electrolyte and fluid retained during AKI, but also because the tubules are recovering from injury and are less responsive to angiotensin/aldosterone/ADH – hence they do not appropriately retain salt and water and the patient may become volume deplete unless they have sufficient intake. A rough rule is to ensure total fluid (oral and iv fluids if necessary) is equal to the urinary volume from the previous day, but this may be reduced if the fluid balance assessment suggests that the patient is overloaded.
Recovery of kidney function after AKI may be incomplete. Poor outcomes are more likely with increasing severity of the insult, prolonged duration of AKI, older patients and those with pre-existing kidney disease.
Further info:
- Patient info on ATN
- Work through some AKI case-based learning (Reources page); then in the Virtual Clinic
- Dialysis in 1959: early dialysis for acute renal failure
- The Korean War establishes a place for dialysis
- The London AKI network has an interesting and useful set of guidelines, policies, teaching resources, and a smartphone App.
- RCPE AKI app is less shiny and shorter, and its content is in a pdf downloadable quite far down that page