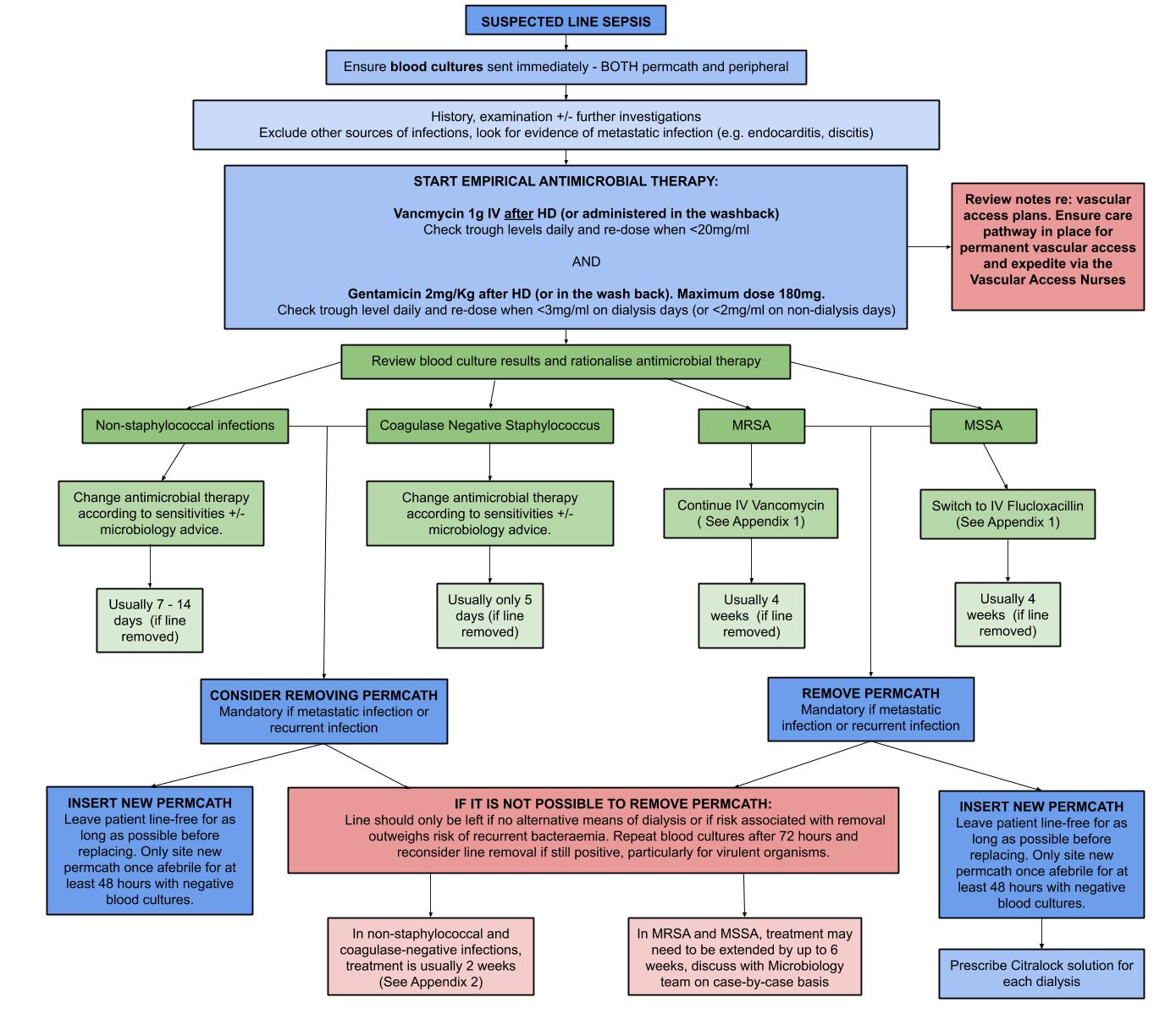
Line Infection Algorithm
Staphylococcus Aureus Infections
Appendix 1
Staphylococcus aureus bacteraemia in dialysis patients is a serious illness with reported mortality up to 30%. Relapse is common, particularly when treatment is inadequate and dialysis lines are not removed. A number of serious complications can arise, including endocarditis, osteomyelitis and discitis. Treat with systemic antibiotics for 4 weeks.
For MRSA empirically use IV vancomycin. Please discuss with microbiology to ensure this is adequate therapy. If MIC is raised, alternative or adjunctive antibiotics may be required.
For MSSA use IV flucloxacillin when possible. Vancomycin is less effective against MSSA than flucloxacillin and substantially increases the risk of treatment failure. If a patient is otherwise suitable for discharge before the treatment course (typically 4 weeks) is completed, consider use of IV flucloxacillin for as long as possible (ideally up to 10 days) whilst the patient remains in hospital, before switching to vancomycin on discharge. When vancomycin is being considered for treatment of MSSA bacteraemia this must be discussed with microbiology to determine whether different or adjunctive antibiotics are indicated.
Cefazolin is sometimes used to facilitate early discharge from hospital.
A critical factor in treating line associated Staphylococcus aureus bacteraemia is removal of the dialysis line in order to prevent relapse of infection and reduce the risk of infective complications. A line should only be kept in situ if removal means that there is no alternative means of dialysis or if risk associated with removal outweighs risk of recurrent bacteraemia and risk of developing deep seated infection (e.g. discitis, osteomyelitis, endocarditis).
If permcath cannot be removed then the patient may need up to 6 weeks of antibiotic therapy; discuss with Microbiology. Repeat blood cultures should be taken after 72 hours of treatment , if they remain positive then permcath should be removed.
When permcaths are removed, ideally leave the patient line free (on antibiotic treatment) for as long as possible before replacing the line. A new permcath should preferably only be inserted after the patient has been afebrile for at least 48 hours with negative repeat blood cultures.
Carefully examine / investigate appropriately for a deep-seated focus of infection, such as endocarditis or discitis. This is particularly relevant for relapsed staphylococcal aureus bacteraemia.
Citralock line lock should be used after a patient has a single episode of staphylococcal aureus bacteraemia related to their dialysis line.
A 14 day course may be considered in patients where the infected dialysis line is removed and fever and bacteraemia resolve within 72 hours of appropriate antibiotic therapy, the patient has no prosthetic intravascular device, there is no clinical evidence of metastatic infection, there is no evidence of endocarditis or thrombophlebitis and the patient is not diabetic or immunosuppressed.
Non-Staphylococcal Infections
Appendix 2
- Coagulase-negative staphylococci (CNS)
Discuss choice of antibiotics with microbiology. Coagulase-negative staphylococci in renal units are not always sensitive to vancomycin. Line infections caused by CNS which are not fully sensitive to vancomycin should be managed with line removal when possible.
If the dialysis line is being replaced then continue antibiotics for 5 days to prevent reinfection of the new line. If the dialysis line is being retained then treat with antibiotics (+/- citralockline lock) for 10-14 days.
- Enterococcus sp.
Remove dialysis line if possible, particularly if no other clear source of bacteraemia apparent and if clinically unwell, persistent bacteraemia, insertion site infection or metastatic complication. Otherwise, it is reasonable to attempt to retain line and treat for 2 weeks with antimicrobial therapy. Discuss choice of antibiotic with microbiology; choice is usually amoxicillin or vancomycin. VRE line infections should always be discussed with microbiology. If dialysis line salvage is being attempted then send repeat blood cultures 48 hours after antibiotics are commenced. If these remain positive then the line should be removed unless no alternative means of dialysis.
- Gram-negative bacilli
Remove line if possible, particularly if no other clear source of bacteraemia (e.g urinary or intra-abdominal) and if clinically unwell, persistent bacteraemia, insertion site infection or metastatic complication. Dialysis lines should always be removed when Pseudomonas aeruginosa or multiresistant Gram-negative organisms are isolated from blood cultures, unless there is no alternative means of dialysis.
The choice of antibiotics is based on identity, sensitivities and discussion with microbiology. If the dialysis line is removed then usually treatment continues for 7-14 days, depending on the underlying source of infection. If unable to remove line then treat with antibiotics for 14 days and use citralock line lock.
If dialysis line salvage is being attempted then send repeat blood cultures 48 hours after antibiotics are commenced. If these remain positive then the dialysis line should be removed unless there are no alternative means of dialysis.
- Yeast (Candida sp.)
Dialysis line should always be removed unless there is no alternative means of dialysis. Repeat blood culture alternate days until first negative blood culture. Treat with antifungal for at least 14 days after line removal or first negative blood culture. Discuss choice of antifungal with microbiology. Arrange ophthalmology review to rule out fungal endophthalmitis.
References
Diagnosis, prevention and treatment of haemodialysis catheter-related bloodstream infections (CRBSI): a position statement of European Renal Best Practice (ERBP). NDT Plus (2010) 3: 234–246
Prevention of Intravascular Catheter-related Infection in Ireland 2010
Guidelines for the Prevention of Intravascular Catheter-Related Infections, CDC 2011
Acknowledgements: Dr Kristjan O. Helgason and Dr Jane Goddard were the main authors for this page. It was first published in January 2012 and updated by Ashley Simpson in November 2020. The last modified date is shown in the footer.