There has been a long history of the dream of replacing defective organs with healthy ones (Craps L,1993). In 1933, the first recorded human cadaveric transplant took place in Russia. The first human kidney transplant from an allograft took place in 1936, by U Voronoy (Starzl TE, 1990). Like all early transplants undertaken before the organ rejection was understood, it failed. In 1954, the first successful kidney transplant between identical twins was performed by the surgeons Joseph.E. Murray and J.Hartwell Harrison in collaboration with the nephrologist J.P. Merrill in the Peter Bent Brigham Hospital in Boston, USA (Starzl TE, 1990). The development of the first useful immunosuppressive drugs permitted the first successful graft from a cadaver to be undertaken in 1962 , opening the door to modern transplantation (Haeger K, 1989; Murray 1992).
Contents
- The first kidney transplant in Edinburgh: twins
- The second kidney transplant: siblings
- The third kidney transplant: father and son
- Early kidney transplants at the Royal Infirmary of Edinburgh
- Nuffield Transplant Surgery Unit at the Western General Hospital (WGH) in Edinburgh
- Kidney donors
- Immunosuppression
- The transplant Unit at the Royal Infirmary of Edinburgh – 1995
The first kidney transplant in Edinburgh: twins
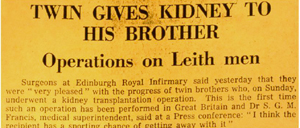
The first successful kidney transplant in UK was performed in Edinburgh by Sir Michael Woodruff and his team on 30th October, 1960. This was a milestone in history of transplantation and the history of the RIE.
On 15th September, 1960, Dr R.F. Robertson referred a 49-year old man suffering from gross impairment of renal function from the Leith Hospital to the RIE. The impairment was suspected to be due to chronic pyelonephritis or chronic glomerulonephritis. The kidney was too small for renal biopsy to be safely performed without ultrasound guidance which was not available in those days. The prognosis for either condition with conventional treatment was poor. It so happened that the patient had a twin brother, who was healthy, and was willing to donate one of his kidneys. The operations were performed on 30th October, 1960 by Sir Michael Woodruff (on the patient) and Mr James A Ross (on the donor).
| “I assisted James Ross, who performed the operation on the donor, and I carried the kidney across to Sir Michael, and then I assisted him. I was a senior registrar at the time.” (Mr B Nolan) |
Following these successful operations, the donor resumed work 3 weeks after the operation; the patient returned to work after 15 weeks (Woodruff et al, 1961). They both lived for a further 6 years before dying from an unrelated disease.
| “The Daily Express reporter bribed the aunts of the twins into saying that he was their nephew, and I was the one who let him visit the twins, thinking that he was family! The following day, photos taken in the patient’s room appeared in the newspaper, and the boss was not very pleased!” (Dr A Lambie) | |
The second kidney transplant: siblings
The second kidney transplant in Edinburgh was carried out between a brother and sister in 1961. The only known way of preventing immunological rejection at the time was total body irradiation. It was discovered in 1956 that if the body was exposed to a large dose of X-radiation, immunological reaction could be reduced (Nolan B, 1985). Therefore in the early days all transplant patients had total body irradiation before the transplant operation. Although the adverse effects of irradiation are known, patients with end-stage renal failure would die very soon without a transplant, so the risks of irradiation and transplantation were considered justifiable for this purpose (Nolan B, 1985). As there was not a Department of Radiotherapy at the RIE, patients had to be transferred to the WGH for irradiation and transferred back to the RIE for the transplant operation. As the patient was very susceptible to infection after total body irradiation, the ambulance also had to be disinfected and “scrubbed out”.
| “The only 2 people who were not carrying Staphylococcus aureus on their skin were Sir Michael (Woodruff) and myself, so we had to go and scrub the ambulance. As you know, Sir Michael was easily irritated, and the whole procedure was rather ‘fraught’!” (Dr A Lambie) |
The result of the second kidney transplant was disappointing. The radiation prevented the kidney from rejection, but the patient died 30 days post-transplant as a result of septicaemia (Woodruff et al, 1962).
The third kidney transplant: father and son
The third kidney transplant in Edinburgh was carried out between a father (donor) and son in April, 1962. By that time, azathioprine (Imuran®), a safer method of immunosuppression than total body irradiation, has been discovered in the USA.
| “Half of the first batch of Imuran® was used in Boston, and the second half was used in Edinburgh”. (Mr B Nolan) |
Therefore the patient transplanted in Edinburgh was the second transplant patient in the world to be treated with azathioprine. It was one of the most successful transplants of all time. The transplanted kidney lasted for more than 20 years (Nolan B, 1985).
Early kidney transplants at the Royal Infirmary of Edinburgh
Early kidney transplants were performed in the surgical theatres of the surgical wards 13 & 14 of the RIE. One surgeon would remove the donor kidney in the anaesthetics room, and carry it to the operating theatre, where the recipient was. A special single-bed unit (room B15) was created for the care of post-transplant patients. The room was converted from an out-patient room which was initially a clinical chemistry room, and located near to the AKU and to Ward 21.
Since the patients of the first renal transplant were identical twins, they did not require immunosuppression. Transplants from non-identical twins requiring whole body irradiation as immunosuppression were anticipated, so after the first transplant, room B15 was modified. It was designed to provide isolation and protection against infection after renal transplant, when the immunosuppressed patients would be very susceptible to infection. As one of the nurses recalled, “7 senior nurses were needed to look after the room in turn!” Sensors were attached to the patient’s body, and were monitored by a nurse, who sat in a room separated from the patient’s room by a glass wall (see plan and account). Within a 24-hour period under normal circumstances, the doctor would only enter the patient’s room once, and the nurse 3 times (Nolan B, 1985). They would take a shower and put on sterile clothing before entering the room.
It was stated in the 1962-63 RIE annual report that ‘8 kidney transplants were performed by Professor Woodruff, who has a suite of rooms in the Department of Therapeutics and works in conjunction with Doctors J.S. Robson and Anne T Lambie’. By 1968, there had been 35 transplants carried out at the single-bed unit of the RIE.
| One of these transplants was well remembered by a surviving patient, who said the following when she was 44 years old (in 2001):
“I was transplanted on 5th January, 1967 when I was nine and a half years old. The kidney was from my mum, and she’s 80 years old now. She’s still healthy. The operation was in the surgical theatre in wards 13 and 14 at the Royal (Infirmary of Edinburgh). I was then put into isolation in room B15 for 5 weeks. I was in one room, and the nurse was in another room. The nurses and doctors had to take a shower before coming into my room, and also take a shower as they go out. They had to put on clean theatre clothes before coming in, and they all wore masks. There was a glass corridor by my room and my mum and dad would watch me from there. They were not allowed into my room. The medical students would come and wave to me behind the glass. They would hold up cards that said “doing well” behind the glass panel. The nurses were in shifts and took turns to look after me. Almost half a dozen of them! I received Imuran and prednisolone for immunosuppression. I did not require dialysis ever again, my kidney has been working for 34 years, and is still going.” |
Visitors from UK and other parts of the world (Europe, USA, Australia, Japan, Burma, Pakistan) came to visit his Sir Michael Woodruff’s department. One of the visitors were Professor Roy Calne from the Department of Surgery at the University of Cambridge who was involved with research on Imuran® with the research group in Boston. Others included J Myburgh who was a leading proponent of transplantation studies in non-human primates.
| Document – A page from the visitors’ book at the Department of Clinical Surgery, RIE, recording visits from around the world, and including Roy Calne and John Humphrey from the UK, and famous names from around the world. View the page (note large size) |
Nuffield Transplant Surgery Unit at the Western General Hospital (WGH) in Edinburgh
The Nuffield Transplantation Surgery Unit was a sophisticated purpose-built unit for transplantation which aimed to provide a “germ-free” environment for transplant patients. It was designed by the architect Peter Womersley to meet the requirements of Professor Woodruff and Dr John Bowie (Senior Bacteriologist, RIE). It was the first custom-built transplant unit in the world, and it became a model for many units that were subsequently built. Professor Woodruff was appointed the Director. The Unit would allow the treatment of 6 patients at any one time, each in a single room in which dialysis and other support could be provided. The building cost of £250,000 was met by the Nuffield Foundation, the staffing and running costs by the Scottish Home and Health Department for the first 5 years, and subsequently by the Regional Hospital Board. It was built at the Western General Hospital as there was no large enough space on the RIE site, and the Department of Radiotherapy at the WGH was convenient for the patients to receive total body irradiation before transplantation. The Nuffield Unit had a corridor (a bridge) that linked to the radiotherapy unit.
| Document – A letter from the secretary to the treasurer regarding the proposed Nuffield Transplantation Surgery Unit at the Western General Hospital. From the Lothian Health Service Archive, with permission. View the letter (note the large size of the page) |
The Unit was officially opened by Sir Peter Medawar, a Nobel Prize winner and the Director of the National Institute of Medical Research on 31 January, 1968. He said Edinburgh has been chosen for the unit because that was where Professor Michael Woodruff, one of the grand masters of the theory and art of transplantation was to be found (Catford EF, 1984).
| “He (Professor Woodruff) is a clinical surgeon who is the first to transplant a kidney in this country. No where in the world will patients get better care.” (Sir Peter Medawar)
“The Nuffield Transplant Surgery Unit was sometimes called ‘Fort Woodruff’, and you can see why from the outside of the building!” (Dr A Lambie) “Lorries keep trying to knock down the bridge, but it’s still standing today” (Dr R Winney) |
| Document – See a plan of the Nuffield Transplant Unit Note: page contains large images |
Dr John L Anderton, a nephrologist in RIE at the time, set up a WGH renal unit which included dialysis, general nephrology, and a transplant follow-up service. The post-transplant facilities at RIE B15 moved to WGH when the Nuffield Transplant Surgery Unit opened in 1968. Professor G.D. Jeffrey Chisholm, Professor of Urology, became the Director of Nuffield Transplant Surgery Unit after Professor Woodruff retired in 1976.

Members of staff at from the Royal Infirmary of Edinburgh and the Nuffield Transplant Surgery Unit at the Western General Hospital, taken in front of the Nuffield Transplant Surgery Unit (1980s). Some of the staff included: Dr Charles Swainson (first left, second row), Elizabeth Sloan (dietician) (fourth left, second row), Dr Robin Winney (third right, second row), Dr John Anderton (first right, second row), Dr Anne Lambie (third left, first row), Pr Jeffrey Chisholm (fifth left, first row). (kindly provided by Sister Sylvia Green)
Between October 1960 and December 1974, 127 patients had renal transplants, and 37 were alive with grafts that had functioned 6 months or more. 28 patients lived more than 2 years, 13 patients more than 5 years, 6 patients more than 8 years and 2 patients more than 12 years. 34 patients were employed, able to do housework, or in full-time education after transplant. 1 patient fathered a child 4 years post-transplant, and 1 patient gave birth 3 years post-transplant. (Woodruff et al, 1976).
By 1981, there were more than 100 patients alive after successful kidney transplantation.
| A patient who was transplanted in 1967 described her memories in 2001:
“I was at the Nuffield Unit 1 year later (after the transplant operation) to have my 2 damaged kidneys out because they were causing my high blood pressure. I remember there were 6 separate rooms, each with a toilet. Each patient was isolated in his or her own room. The room was separated from the corridor with a glass panel, and there’s a microphone where you can speak through, but everyone can hear your conversation! There were these holes in the glass panels where the lines of the dialysis machines were fed through.” |
Kidney donors
In the 1960s kidneys for transplant operations came from living donations. When cadaveric transplants became more acceptable in later years, the number of living donors reduced. After some time, the number of living donors increased again when there was a shortage of cadaveric donors.
| Donor | Number |
| Identical twin | 2 |
| Living relative (not twin) | 22 |
| Unrelated living donor | 2 |
| Cadaver | 101 |
Origin of kidneys for the first 127 transplants (to the end of 1974) (Woodruff et al, 1976)
The first kidney transplant was performed between twins, and no immunosuppression was required. It was a successful operation. Later transplantations between family members or cadaveric donors were not as successful. This may be attributed to the side effects of total body irradiation before azathioprine became available. Moreover, the quality of the kidneys from cadaveric donors was not very good since ventilators were not routinely used to ventilate the donors at the time. Therefore the kidneys may have been anoxic for some time before they were retrieved in a side room. Now organ retrieval is undertaken in an operating theatre, where the deceased is being ventilated. The UK criteria for brain stem death were published in 1976. This allowed heart-beating donations, which transformed transplantation.
Immunosuppression
Total body irradiation was employed from 1956 to reduce graft rejection. However, irradiation could lead to destruction of the nervous system, fluid loss and bacterial invasion, and could cause death within a few hours to a few days.
In 1959, 6-mercaptopurine was discovered. It was a very toxic drug but protected kidney grafts in dogs. In 1962, R.Y. Calne and J.E. Murray reported the successful use of azathioprine, a derivative of 6-mercaptopurine, on a kidney transplant patient in Boston, USA (Haeger K, 1989). The second half of this first batch of azathioprine was used in a successful renal transplantation in Edinburgh in the same year. Azathioprine is converted to a purine antagonist and inhibits DNA synthesis, reducing immune function.
In 1961, Calne, Peart and Porter launched a transplantation programme using azathioprine and corticosteroids. In April 1962, two episodes of rejection after a cadaveric kidney transplant in Boston were treated with azathioprine and cortisone. The combination of azathioprine and corticosteroids became the basic immunosuppressive regime for many years (Kuss R, 1992).
In 1951, Sir Michael Woodruff published a paper on his work on anti-lymphocytic serum (ALS) in the rat (Woodruff & Forman, 1951). He modified the method used by Cruickshank in 1941 and produced rabbit-anti-rat ALS which was used in black-and-white hooded rats to induce lymphopaenia. This was a serum against “immunocompetent” lymphocytes, a more specific biological method to suppress the immune system by acting directly on the lymphocytes. The ALS was used in experiments only on rats at first. He continued this work in Edinburgh in the 1960s, where he found that lymph drainage and administration of ALS resulted in prolonged homograft survival in rats, where the maximum effect was achieved with treatment both before and after graft transplantation (Woodruff & Anderson, 1963). In 1966, Sir Michael Woodruff and colleagues showed that ALS against dog thoracic lymphocytes prolonged the survival of whole kidney homotransplants in dogs. Sir Michael Woodruff and his team made anti-lymphocyte globulins (ALG) and ALS in collaboration with colleagues at the Royal (Dick) School of Veterinary Science in Edinburgh. Theses polyclonal antibodies were made in horses.
This work on ALS began to attract the attention of other scientists, including Sir Peter Medawar in London, Paul Russell and Tom Starzl in the USA.
 |
An ampoule of anti-human-lymphocyte globulins produced by Sir Michael Woodruff, Professor Keith James and colleagues in 1972 (courtesy of Professor Keith James) |
Understanding of the ALG was important if it were later to be used clinically on humans, and Keith James and Sir Michael Woodruff undertook extensive research to establish this. The team investigated the mode of action of ALG, the kinds of immune response which it suppressed, and the nature of the molecular characteristics of the antibody (James K, 1967). ALG was found to be predominantly of the IgG class. Moreover, the intact IgG was needed to give a biological effect. Antibody fragments, F(ab’)2 or Fab, did not work since they did not fix complement, and could not lead to complement-mediated lysis of lymphocytes (James K, 1967). ALG also suppressed antibody formation experimentally (James & Jubb, 1967). This suppression depended on the antigen, the species of rat or mouse and the timing of antigen challenge (ALG was inject before antigen challenge to give immunosuppression). ALG was later used in humans, soon after the Nuffield Transplant Surgical Unit opened. ALG was used as an adjunct to other immunosuppressants, and it was observed that grafts were functioning after 5 years in 4 out of 14 renal transplant patients who received ALG in addition to azathioprine and prednisolone (Woodruff et al, 1976).
The key studies on the graft enhancing effect of prior transfusion of donor blood in rodents were performed by Mr A McL Jenkins and Sir MFA Woodruff in the early 1970s (Woodruff & van Rood, 1983; A McL Jenkins Master of Surgery Thesis 1972/73). In 1976, Paul Terasaki demonstrated that long-term prognosis in humans post-transplant was directly related to the number of pre-transplant transfusions (Kuss R, 1992). It was thought that blood transfusion enhanced graft survival, through an unknown mechanism.
| “In Belfast, all the pre-transplant patients were transfused, and they had the best results. Edinburgh was anti-transfusion due to the hepatitis outbreak.” Dr R Winney |
In the blood transfusion, only frozen washed red cells were used (the blood was leucocyte-depleted). Later on, there was more evidence that blood transfusion enhanced graft survival, possibly by inducing tolerance. After a while, it became the usual practice in Edinburgh to transfuse 4 units of blood before transplant. It was shown that blood transfusion together with a low-dose steroid regime increased the 3-year graft survival rate from less than 40% to 66% (Notghi et al, 1986). Reductions in acute rejection reduced the numerous side effects associated with high steroid intake, including mortality and bone morbidity. However, transfusion was not without problems: some patients became highly sensitised to transplant antigens, making transplantation very difficult. After the introduction of the more effective anti-rejection agent cyclosporin, pre-transplant transfusions were abandoned.
More recent immunosuppressants include FK506 (tacrolimus), rapamycin (sirolimus), mycophenolate mofetil (MMF), and monoclonal antibodies against lymphocytes, a more specific form of the polyclonal antibodies that Professor Woodruff set out to make. Cyclosporin A, tacrolimus and sirolimus work by inhibiting cytokine-driven T-lymphocyte signalling, affecting their proliferation, maturation and trafficking. MMF has a more selective mode of action than azathioprine, it inhibits T-lymphocyte and B-lymphocyte proliferation. Monoclonal antibodies such as basiliximab and daclizumab prevent T-lymphocyte proliferation.
The transplant Unit at the Royal Infirmary of Edinburgh – 1995
The Nuffield Transplant Surgery Unit at WGH and Scottish Liver Transplant Unit at RIE joined to form the “Transplant Unit of the RIE” on the 5th June 1995, combining the efforts of the transplant surgeons, doctors, nurses and other staff. The WGH dialysis unit became a satellite unit of the RIE for dialysis, with 9 patients a day, initially with 2 shifts per day and a clinic at the WGH. The workload of the renal unit increased during early days of liver transplants, since they were associated with a high incidence of acute renal failure.
In the year between between April 2000 and March 2001, 64 renal transplants were performed. The one-year graft survival is 95%. This compares with 37 out of 127 patients alive with grafts functioning more than 6 months between October 1960 and December 1974 (Woodruff et al, 1976).
Read pages about the Transplant Unit today
 |
 |
| The entrance to the Transplant Unit at the very top of the Royal Infirmary of Edinburgh, 2001 | |