
You are the FY1 on the MAU . You are called from the laboratory about some unexpected blood results from a gentleman who is on your ward.
You quickly scribble them down on a post-it to give you time to process what this means.
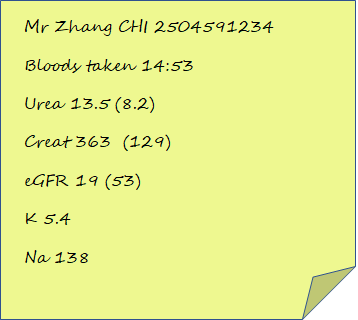
What do you want to do now?
You need to know the context of these blood tests and why they were taken. You have a look on Trak and see that Mr Zhang was admitted with general lethargy, mild fever and just generally unwell. He had been investigated by his GP who found that his kidney function was a little deranged but identified no infectious source. He has underlying chronic renal disease which is thought to be linked to un-controlled blood pressure in the past. The blood tests were a routine admission.
Whilst potassium is a little high, you could probably monitor it at this level. It would be good to get an ECG to check there is no abnormality there and this would help you decide if you needed to treat it at this level.
Remember Mr Zhang has just had an MI and is likely to have been started on quite a few new medications for secondary prevention. Have a think about what medications could cause renal impairment post-MI.
This is rarely a wrong answer and whilst unexpected blood tests can be a sign of something wrong, without seeing the patient it is difficult to have a meaningful interpretation of these. Remember treat the patient not just the numbers!
Whilst this may be part of your management plan, I think there is a little more information that should be gathered prior to ringing them for advice.
So what do you find out – click reveal to find out information about Mr Zhang.
PC – Generally unwell and abnormal renal function
HPC – Feeling generally unwell following MI 4 weeks ago. Had been well following discharge and felt like was progressing slowly however for last 2 weeks has had general malaise, mild myalgia and feeling a little feverish. No infective symptoms. No chest pain, SoB. No cough or coronavirus contact.
PMHx – Hypertension, hypercholesterolaemia, COPD, MI- 2x stents to LAD
Medications
Lisinopril 10mg od
Amlodipine 10mg od
Bisoprolol 2.5mg od
Aspirin 75mg od
Clopidogrel 75mg od
Salbutamol inhaler prn
Atorvastatin 40mg od
Trellegy 1 inh/day
Allergies – penicillin
PMHx – Father MI in 50’s. Mother – vascular dementia
Social – Smokes 20 a day for 40 years, drinks 5 pints 5 nights a week, retired, lives sedentary lifestyle.
You go to see the patient
Feeling a bit nauseous, no chest pain. Alert, eating and drinking
- A- Maintaining own
- B – Chest hyperinflated, mild creps bilaterally AE, Sats 89% RA – Normal for patient, No increased WoB
- C- Warm peripherally, HS 1+2+0 nil added sounds. BP 115/63, HR 65, pulses palpable, no radio/radio delay. No bruits, no sacral oedema, no peripheral oedema, JVP not visible, mucus membranes moist
- D- Temp 37.8, Abdo soft no organomegaly, passing urine
Bloods – Hb 135, WCC 10.7, eosinophils 0.55 x 109 /l , Plt 258 CRP 15
CXR mild bilateral pleural effusions
Allergy – there is some signs of inflammation and eosinophillia so this is a possibility
Infections – there is mild pyrexia and high normal WCC, although there is no sign of sepsis it wouldn’t be impossible he had an infection
AKI – Secondary to ACE-Inhibitor introduction/Uptitration. We would need to know if he was already being treated with ACE-inhibitor prior to his MI
AKI – related to contrast nephropathy – usually occurs closer to time of contrast exposure but is a possibility
You are about to go and get some help because you are unsure as to what exactly is going on with this gentleman when the nurse asks you – Have you seen the rash on his foot.
You go to have a look

Rash is present bilaterally, feet are cool peripherally. neurovascularly intact
What is this and does this change your differential diagnosis?
You call the med reg as your SHO is busy with another sick person. Write your referral as a structured SBAR and compare with the one below.
Click on SBAR to reveal
S- 61 year old gentleman with new acute on chronic kidney injury, creatinine of 363 and eGFR of 19, potassium is safe. He also has myalgia and pyrexia. No coronavirus contacts.
B- Recent MI and angiography with 2x stents inserted, hypertension and hypercholesterolaemia. Strong family history of vascular disease.
A – He is alert and well. Euvolaemic in terms of fluid balance. He has no cardiovascular or GI abnormalities. His respiratory exam is largely normal but he does have small bilateral pleural effusions. He has a mildly elevated temp at 37.8. He also has a mottled legs bilaterally which are cool but neurovascularly intact
R – I would like you to come and see the patient and give me some advice on their management.
After your brilliant referral, the registrar comes to see the patient with you.
He advises that we should organise a renal ultrasound and refer this gentleman to the renal team as his renal impairment may not be reversible.
What do you think the likely diagnosis is?
Click diagnosis to reveal
Cholesterol embolisation from angiography
Well done you have completed the case.
