Contents
Hyperkalaemia in the community
Hyperkalaemia detected in the community is a frequent reason for referral to secondary care. These pages are designed to assist decision-making in primary care. We also have guidance on management of hyperkalaemia in hospital.
Expert guidelines
1) Treatment of acute hyperkalaemia in adults (July 2020): the UK Renal Association Clinical Practice Guideline. This gives very comprehensive advice on hyperkalaemia (is 161 pages long). The flow-chart on p156 on “Management of Hyperkalaemia in the Community” recommends a simple management algorithm.
2) ‘Change in renal function associated with drug treatment in heart failure: national guidance (January 2019)’ . These joint cardiology-renal guidelines specifically address patients with heart failure (in whom there may be a strong rationale to continue renin-angiotensin inhibitors). Table 2 gives a suggested management algorithm.
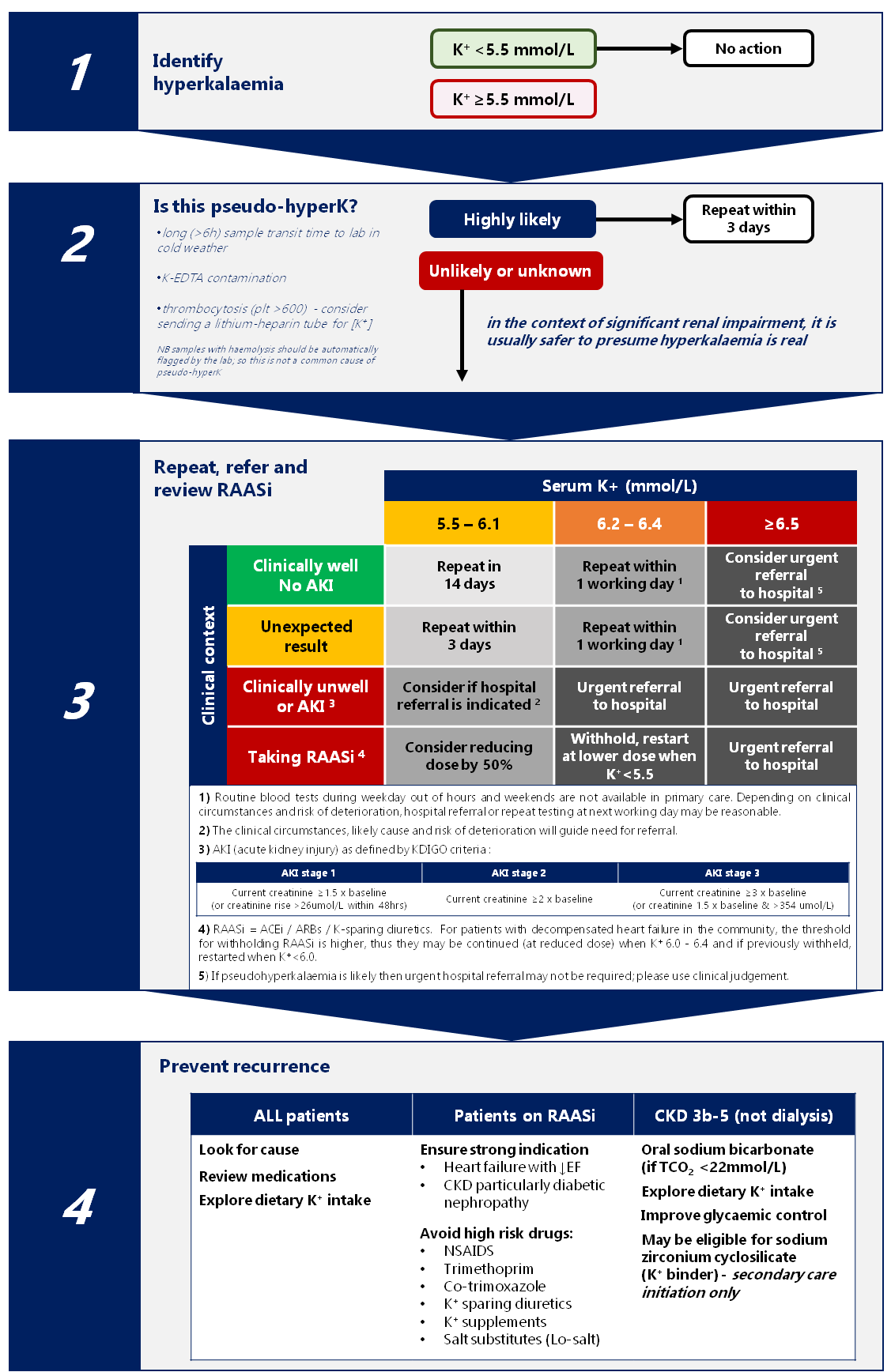
Our recommendations for the management of hyperkalaemia in primary care:
Based on our experience of referrals from primary care, we have used the relevant recommendations from these expert guidelines to help answer the most commonly asked questions:
- Should this patient come to hospital for assessment and treatment?
- If they don’t need to come to hospital, when should the potassium be re-checked?
- Should renin-angiotensin-aldosterone system inhibitors be stopped?
- What other factors should be addressed to prevent recurrence?
Suggested management algorithm:
Most patients requiring urgent assessment in hospital should be referred to acute medicine or the emergency department using standard referral pathways. (Patients with pre-existing advanced CKD or heart failure may referred to the nephrology or cardiology teams but will often have to be admitted via acute medicine.)
Notes and rationale:
The most important principles are:
- the risk factors for hyperkalaemia are renal failure (AKI or CKD), RASi, potassium-sparing diuretics, heart failure, diabetes and adrenal insufficiency
- therefore dangerous hyperkalaemia is almost never encountered in patients with normal renal and adrenal function who are not taking renin-angiotensin-aldosterone inhibitors (RAASi) or potassium-sparing diuretics
- patients with heart failure with reduced ejection fraction (HFrEF) and diabetic kidney disease with heavy albuminuria (uACR > 30 mg/mmol) stand to benefit a lot from ACEi/ARBs and therefore it may be worth deploying strategies to allow these medications to be continued (e.g. dietary K restriction, K binders, co-prescription of loop or thiazide diuretics)
- patients with other proteinuric kidney disease (e.g. diabetes and uACR > 3 mg/mmol or no diabetes and uACR > 30), vascular disease and stroke are also likely to benefit from ACEi/ARBs but to a lesser extent (i.e. the NNT to prevent important outcomes will be higher than in HFrEF and diabetic nephropathy)
- have a low threshold for discussing with the relevant team in secondary care (e.g. heart failure team or renal team)
Drugs that can predispose to hyperkalaemia include:
- RAASi: including ACE inhibitors (ACEi), angiotensin receptor antagonists (ARBs), angiotensin receptor-neprilysin inhibitors (ARNI) and mineralocorticoid receptor antagonists (MRA)
- potassium-sparing diuretics (e.g. amiloride / spironolactone)
- trimethoprim (also in co-trimoxazole)
- non-selective beta-blockers
- heparin
Our guidance on the use of sodium zirconium cyclosilicate (Lokelma) is given here. Patients may be eligible if they have CKD3B or worse, significant proteinuria (uPCR > 50 mg/mmol) and attend a renal outpatient clinic. Lokelma may then be prescribed to facilitate use of RAASi; there are defined criteria in the guideance for determining whether hyperkalaemia is currently preventing RAASi from being used at therapeutic doses.
Advice on dietary potassium restriction can be found here.
Acknowledgements
This page was first written by Tariq Farrah (January 2021). Date and time of most recent edit is shown in the footer.